ventilationwww.zhiboba.com
BritishMedicalAssociationbma.
org.
ukCOVID-19–ethicalissues.
AguidancenoteInbriefDuringthispandemic,doctorsareworkingunderextremepressure.
Manyarebeingdivertedintonewandunfamiliarareasofworkandfindingthemselvesworkingatorevenbeyondtheordinarylimitsoftheircompetenceorexpertise.
Retireddoctorsarereturningtopractice,andfinalyearmedicalstudentsarebeingfast-trackedintofront-lineroles.
Resourcesarebecomingincreasinglyrestrictedandchoicesofavailablecarelimited.
Thepandemicisfast-moving,relativelyunpredictableandofuncertainduration.
Providingcaretoexistingstandardsislikelytobedifficult.
Wheretheybecomenecessary,prioritisationandtriagedecisionswillbeprofessionallychallenging.
Doctorswillunderstandablybeconcernedabouttheirabilitytoprovidesafeandethicalcare,andtheirownhealthandsafetyaswellasthoseoftheirfamilyandfriends.
Theywillalsobeconcernedthattheiractionsmayattractcriminal,civilorprofessionalliability.
Thisguidancenoteaddressessomeofthemainethicalchallengeslikelytoariseduringthispandemic.
Whereverpossible,linkstoothersourcesofadviceareprovided.
Fromanethicalandprofessionalregulatoryperspective–whichisalsolikelytogoverntheapproachoftheCourtsifthereareanylegalchallenges–doctorsshouldbereassuredthattheyareextremelyunlikelytobecriticisedforthecaretheyprovideduringthepandemicwheredecisionsare:––reasonableinthecircumstances––basedonthebestevidenceavailableatthetime––madeinaccordancewithgovernment,NHSoremployerguidance––madeascollaborativelyaspossible––designedtopromotesafeandeffectivepatientcareasfaraspossibleinthecircumstances.
Shoulddecisionsbecalledintoquestionatalaterday,theywillbejudgedbythefactsavailableatthetimeofthedecision,notwiththebenefitofhindsight.
IntroductionandbackgroundWeareintheearlystagesofapandemicoutbreakofCOVID-19,forwhichwecurrentlyhavenoeffectivevaccineandverylittletreatment.
1Basedoncurrent–imperfect–knowledge,COVID-19hasamortalitypercaseratioofsomewherebetween0.
5and3.
4%,2althoughthesefiguresarelikelytoberevisedoncemoreisknownaboutbackgroundinfectionrates.
AninformedestimatebytheEnglishChiefMedicalOfficer(CMO)ProfessorChrisWhittysuggestsaprobablemortalityrateintheregionof1%orless.
3Othercommentatorssuggestitmaybesignificantlyhigherthanthis,although1https://www.
bbc.
co.
uk/news/world-51839944.
Accessed12Mar.
20.
2https://www.
who.
int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---3-march-2020.
Accessed12March20203https://www.
theguardian.
com/world/2020/mar/06/uk-has-plans-to-deal-with-pandemic-causing-up-to-315000-deaths.
Accessed12Mar.
20.
2itistooearlytomakedefinitivestatements.
(Bycomparison,seasonalfluhasamortalityrateintheregionof0.
1%.
)Currentdatasuggestthatthosemostatriskincludethoseover70andthosewithunderlyingco-morbidities,withmenbeingathigherriskthanwomen.
COVID-19islikelytoaffectalargeproportionofthepopulation.
Itisalreadycreatingsignificantpersonalandeconomicdisruptionandloss.
Giventhatitmaylastseveralyears,sustainedpressurewillcontinuetobeplacedonessentialservicessuchashealth,energy,foodandpharmaceuticalproductionanddistribution,watersupplyandwastedisposal.
Giventhelackofpre-existingimmunity,itislikelythataconsiderablepercentageofthepopulationwillseek,andmayatsomepointrequire,medicalattention.
ThereislittleornosurgecapacityintheNHSalthoughvigorousattemptsarebeingmadetoreducedemandthroughsocialdistancingandtoincreasetheavailabilityofintensivecarebeds.
Nevertheless,itispossiblethatserioushealthneedsmayoutstripavailabilityanddifficultdecisionswillberequiredabouthowtodistributescarcelifesavingresources.
Althoughweprofoundlyhopethiswillnotbehappen,itisimportantthatwebegintothinknowabouthowwewouldrespondshouldthatsituationariseinthefuture.
Todate,muchofthefocushasbeenonconventionalpublichealthtoolsforthemanagementoftheearlystagesofanoutbreak,suchasquarantineandotherformsofsocialdistancing.
Asthepandemicdevelopsandhealthservicesareputundergreaterpressure,itispossiblethatdecisionsabouttheallocationofpotentiallylife-savingtreatmenttoindividualpatientswillfalltohealthcareprovidersandindividualhealthprofessionals.
Thiswouldgiverisetosearchingethical–andprocedural–questionsanditistothoseandrelatedissueswenowturn.
Anethicalframework4Therehasalwaysbeenanethicaltensioninmedicinebetweenadoctor'sconcernforthehealthandwelfareoftheindividualpatientandconcernforthehealthofpopulations.
Indangerouspandemicstheethicalbalanceofalldoctorsandhealthcareworkersmustshifttowardstheutilitarianobjectiveofequitableconcernforall–whilemaintainingrespectforallas'endsinthemselves'.
Priortothe2009pandemic,theGovernmentissuedanethicalframework–revisedin2017–designedtohelppeoplethinkthroughstrategicaspectsofdecision-makingduringapandemic,aswellasprovidinganethicalcompassforclinicians.
Ittooktheformofseveralguidingprincipleswhicharesetoutbrieflybelow.
––Equalrespect:everyonemattersandeveryonemattersequally,butthisdoesnotmeanthateveryonewillbetreatedthesame––Respect:keeppeopleasinformedaspossible;givepeoplethechancetoexpresstheirviewsonmattersthataffectthem;respectpeople'spersonalchoicesaboutcareandtreatment––Minimisetheharmofthepandemic:reducespread,minimisedisruption,learnwhatworks––Fairness:everyonemattersequally.
Peoplewithanequalchanceofbenefitingfromaresourceshouldhaveanequalchanceofreceivingit–althoughitisnotunfairtoaskpeopletowaitiftheycouldgetthesamebenefitlater––Workingtogether:weneedtosupporteachother,takeresponsibilityforourownbehaviourandshareinformationappropriately––Reciprocity:thosewhotakeonincreasedburdensshouldbesupportedindoingso––Keepingthingsinproportion:informationcommunicatedmustbeproportionatetotherisks;restrictionsonrightsmustbeproportionatetothegoals––Flexibility:plansmustbeadaptabletochangingcircumstances––Openandtransparentdecision-making:gooddecisionswillbeasinclusive,transparentandreasonableaspossible.
Theyshouldberational,evidence-based,theresultofareasonableprocessandpracticalinthecircumstances.
Resourceallocation4Thefollowingethicalframeworkistakenfromhttps://www.
gov.
uk/guidance/pandemic-flu#ethical-framework.
Accessed13Mar20.
Duringthispandemic,itispossiblethatdemandonhealthservicesmayoutstriptheabilityoftheNHStodeliverservicestopre-pandemicstandards.
AswehaveseeninChina,ItalyandSpain,deathsfrequentlyfollowhospitalisationandcriticalcareinterventions.
InWuhan,5%ofthoseinfectedwereadmittedtoICU,and2.
5%requiredmechanicalventilation.
5Itispossiblethereforethatrestrictionsintheavailabilityofmechanicalventilationmayforaperiodbecomesevere.
Althoughnoteveryonewillbecomeillatonce,theinitialwaveofillnesscanbeextremelyrapid,overafewdaystoafewweeks.
Inthesecircumstances,ifdemandoutstripstheabilitytodelivertoexistingstandards,morestrictlyutilitarianconsiderationswillhavetobeapplied,anddecisionsabouthowtomeetindividualneedwillgivewaytodecisionsabouthowtomaximiseoverallbenefit.
Weknowthathealthprofessionalswouldfinddecision-makinginthesecircumstancesethicallychallenging.
Suchextremesituationsbringaboutatransformationofdoctors'everydaymoralintuitions.
Theobligationtopersevereinthefaceofanextremelyillpatientwouldbechallengedbyquantitativedecisionsbasedonmaximisingtheoverallreductionofmortalityandmorbidity,andtheneedtomaintainvitalsocialfunctions.
Doctorswouldbeobligedtoimplementdecision-makingpolicieswhichmeansomepatientsmaybedeniedintensiveformsoftreatmentthattheywouldhavereceivedoutsideapandemic.
Healthprofessionalsmaybeobligedtowithdrawtreatmentfromsomepatientstoenabletreatmentofotherpatientswithahighersurvivalprobability.
Thismayinvolvewithdrawingtreatmentfromanindividualwhoisstableorevenimprovingbutwhoseobjectiveassessmentindicatesaworseprognosisthananotherpatientwhorequiresthesameresource.
Althoughdoctorswouldlikelyfindthesedecisionsdifficult,ifthereisradicallyreducedcapacitytomeetallserioushealthneeds,itisbothlawfulandethicalforadoctor,followingappropriateprioritisationpolicies,torefusesomeonepotentiallylife-savingtreatmentwheresomeoneelsehasahigherpriorityfortheavailabletreatment.
Thesearegravedecisions,butthelegalprincipleswereestablishedinrelationtotheallocationoforgansfortransplantationandhavebeenrecentlyupheldbytheCourtofAppeal.
6Inrelationtoadultslackingcapacity,theseprioritisationdecisionsarenot'bestinterests'decisionsundercapacitylegislation.
Thefactthatapatientlackscapacitydoesnotimporta'bestinterests'decision-makingmodel.
Inshort,thereisnoautomaticpriorityforthosewholackcapacityanddecisionsabouttheirtreatmentshouldbemadeinthesamewayasforallotherpatientsrequiringtreatment.
IfthereisaneedtolimittheavailabilityofintensivecareforpatientsbecauseoftheCOVID-19pandemicandacriticalshortfallinICUcapacity,itwouldbeunethicaltoapplythoselimitsdifferentlytopatientswithorwithoutappointedsurrogatedecision-makersorthosewithorwithoutparticularreligiousviews.
Itisessentialthat,shouldtheyberequiredto,doctorsmakethesedecisionsinaccordancewithdecision-makingprotocolsrolledoutbyemployingorcommissioningorganisations.
Thiswouldneedtobebothpracticalandsufficientlyflexibletorespondinatimelymannertouncertaintyandrapidlychangingcircumstances.
Alldecisionsconcerningresourceallocationmustbe:––reasonableinthecircumstances––basedonthebestavailableclinicaldataandopinion––basedoncoherentethicalprinciplesandreasoning––agreedoninadvancewherepracticable,whilerecognisingthatdecisionsmayneedtoberapidlyrevisedinchangingcircumstances––consistentbetweendifferentprofessionalsasfaraspossible––communicatedopenlyandtransparently––subjecttomodificationandreviewasthesituationdevelops.
Whereadecisionismadetowithholdorwithdrawsomeformsoftreatmentfrompatientsonthegroundsofresourceallocation,itiscrucialthatthosepatientsstillreceivecompassionateanddedicatedmedicalcareandattention,asfaraspossibleinthecircumstances.
Thisshouldincludeappropriatesymptommanagementand,wherepatientsaredying,thebestavailableend-of-lifecare.
Ifitbecomesnecessarytomakethesedecisions,theyarelikelytohaveasignificantemotionalimpactonhealthworkers,bothintheshorttermand,insomecases,moreenduringly.
Such5https://www.
nejm.
org/doi/full/10.
1056/NEJMoa2002032.
6SeeR(BA)vTheSecretaryofStateforHealthandSocialCare[2018]EWCACiv2696.
34decisionsmayadverselyaffectthefamilyandfriendsofhealthcarestaff.
Doctorsandotherfrontlinehealthworkersarealreadyoverstretched,andtheabilityofthehealthsystemtorespondtothepandemicwillbedependentupontheirwellbeing.
Itisessentialthatemployerstakestepstoprovideappropriatesupport,includingclinicalethicscommitteesupportandpsychologicalsupport,toallhealthprofessionalsworkingduringthepandemic,manyofwhommayfindworkingintheunfamiliarandstrenuousconditionsofapandemicbothpracticallydifficultandmorallyandemotionallychallenging.
Itisessentialthattheirwellbeingisprioritised,bothforitsownsakeandaspartofmaintainingeffectiveclinicalservices.
Healthprofessionalsshouldseektoensuretheirownwellbeing,andthewellbeingoftheircolleaguesasfaraspossibleinthecircumstances.
Itisvitalthatallthoseworkinginhealthsystemsendeavourtoworkcollaborativelyandsupportivelybothwithinteamsandmorewidely.
TriageIfservicesareoverwhelmedduringthispandemic,healthproviderswillputinplace–orexpand–systemsoftriage.
Triageisaformofrationingorallocationofscarceresourcesundercriticaloremergencycircumstanceswheredecisionsaboutwhoshouldreceivetreatmentmustbemadeimmediatelybecausemoreindividualshavelife-threateningconditionsthancanbetreatedatonce.
Triagesortsorgradespersonsaccordingtotheirneedsandtheprobableoutcomesofintervention.
Itcanalsoinvolveidentifyingthosewhoaresoillorbadlyinjuredthatevenwithaggressivetreatmenttheyareunlikelytosurviveandshouldthereforereceivealowerpriorityforacuteemergencyinterventionswhilenonethelessreceivingthebestavailablesymptomaticrelief.
Itispossiblewecouldreachapointwherethedecisionsmadeintriagewilldeterminewhetherpotentiallylargenumbersofindividualswillreceivelife-savingtreatmentornot.
Itisessentialthereforethattheprinciplesunderlyingthedecisionsaresystematicallyapplied.
Inthesecircumstancesitislikelythatprioritywillordinarilybegiventothosewhoseconditionsarethemosturgent,theleastcomplex,andwhoarelikelytolivethelongest,therebymaximisingoverallbenefitintermsofreducedmortalityandmorbidity.
Prioritydecisionswillbedependentupontherelationshipbetweentheavailabilityofresourcesandthedemand.
Ifseriousdepletionofresourcesarises,decisionsaboutwhichpatientsshouldreceivetreatmentwillchangeoverthecourseofthepandemic.
WeknowthatcurrentdataaboutCOVID-19showastrongcorrelationbetweenolderageandmortality.
Althoughworkhasnotbeendoneyettoestablishwhetherthisreflectsanactualeffectofage,orsimplyacorrelationbetweenageandco-morbiditiesthatwillaffectsurvivalrates,itislikelythatthemostchallengingtriagedecisionswillbemadeforthesegroups.
Iftheybecomenecessary,thesedecisionsmustnotbesolelybasedonage.
Ethically,triagerequiresidentificationofclinicallyrelevantfactsaboutindividualpatientsandtheirlikelihoodofbenefitingfromavailableresources.
Youngerpatientswillnotautomaticallybeprioritisedoverolderones.
Apandemicwillobviouslynotpreventpeoplebeingillinotherways.
TriagedecisionswillthereforenotonlyrelatetothosepatientsdirectlysufferingfromCOVID-19.
Similarcriteriawillneedtobeappliedtoallvarietiesofmedicalneed.
Consequently,thresholdsforgrantingaccessto,forexample,intensivecareorventilationwillhavetobechangedforallpatientswithallpresentingcriteria.
Byitself,infectionwithCOVID-19shouldnotguaranteepriority.
Thepresenceofco-morbiditymayexcludeindividualsfromeligibility.
Inthesecircumstances,itmaybenecessarytodiscontinuetreatmentthathasalreadybeenstarted,astherearepatientsinneedwhoseoutcomesarelikelytobemorefavourable.
Difficultdecisionswillarisewherestrenuousinterventioncouldreducemortalitysignificantlybutwouldmeanthatindividualpatientsuseresourcesthatcouldleadtobetteroutcomesforalargernumberofotherpatients.
Thepandemic,andtherestrictedavailabilityofintensivecare,willinfluenceotherclinicaldecision-makingwithinthehospital.
Forexample,itwillbeimportantforclinicianstoreviewanddocumenttheappropriatenessofcardiopulmonaryresuscitationforallinpatients(withorwithoutCOVID-19associatedillness)wherethereisapossibilityofacutedeterioration.
Ifpatientshavesufficientbackgroundillness,co-morbidityand/orfrailtythattheywouldnotbeadmittedtointensivecare(becauseofthenecessaryrestrictionsonadmissions),itisimportantthatcardio-pulmonary5resuscitationisnotcommencedintheeventofacollapse.
Performingadvancedresuscitationforapatientforwhompost-resuscitationintensivecarecannotbeprovidedwouldpotentiallycauseharmtothepatient,consumelimitedresourcesatatimeofconsiderablestrain,andpotentiallyputtheresuscitationteamatunnecessarypersonalrisk.
ACHESTconsensusstatementontriageandcareofthecriticallyillduringpandemicsanddisasterscanbefoundhere:https://journal.
chestnet.
org/article/S0012-3692(15)51990-9/pdfAusefulBMJcommentontriageduringtheCOVID-19outbreakcanbefoundhere:https://blogs.
bmj.
com/bmj/2020/03/09/covid-19-triage-in-a-pandemic-is-even-thornier-than-you-might-think/MedicalutilityThefocusofhealthprofessionals'attentionduringtriagewillbeondeliveringthegreatestmedicalbenefittothegreatestnumberofpeople.
Behindsuchadeceptivelysimpleprinciplelurkchallengingdecisions.
Suchastrategyrequiresanepidemiologicaljudgmentaboutat-riskgroupsthatwillvaryaccordingtotheepidemiologyofthedisease.
Tomaximisebenefitfromadmissiontointensivecare,itwillbenecessarytoadoptathresholdforadmissiontointensivecareoruseofscarceintensivetreatmentssuchasmechanicalventilationorextracorporealmembraneoxygenation.
Relevantfactorspredictingsurvivalincludeseverityofacuteillness,presenceandseverityofco-morbidityand,whereclinicallyrelevant,patientage.
7Thosepatientswhoseprobabilityofdying,orofrequiringaprolongeddurationofintensivesupport,exceedsathresholdlevelwouldnotbeconsideredforintensivetreatment,thoughofcoursetheyshouldstillreceiveotherformsofmedicalcare.
Thedifficultywilllieinapplyingthegeneralprinciplestoacomplex,unpredictableandevolvinghealthcrisisofuncertaindurationandextent.
Ethicalquestionsarelikelytoarise,however,wheretherequirementsofmedicalutilityhavebeenmet,butchoicesbetweenindividualswithequalneedstillhavetobemade.
OnelikelychallengeduringthecurrentpandemicisthatlargenumbersofpeoplerequiringintensivecarearelikelytohavesimilarchancesofsurvivalandanticipatedlengthsofstayinICU.
Inthesecircumstances,considerationwillhavetobegiventoanegalitarianapproachthatensuresafairdistributionofresources.
Themostlikelyapproachinthefirstinstanceisamodifiedqueuingsystem,basedonthewell-establishedandunderstoodprincipleof'firstcome,firstserved'.
Thiswouldmeanthatthosepatientswhobecomecriticallyillearlierinthepandemicwouldbemorelikelytobeadmittedtointensivecareorreceivemechanicalventilationthanthosewhobecomesimilarlyillatalaterstage,albeittheymayonlybeofferedintensivesupportforadefinedbutlimitedperiod.
Whilesuchanapproachisprocedurallysimpletoapply,andarguablyfair,itisnotwithoutitschallenges.
Itis,forexample,likelytogiveprioritytothosewhoaremobile,whohaveaccesstotransport,orwholiveclosetohospitalsandothersitesofhealthprovision.
WithdrawingorwithholdingtreatmentThereislikelytobesignificantethicalattentiontodecisionsaboutwithholdingtherapiesfrompatientsatthetimeofdeterioration.
However,thereisnoethicallysignificantdifferencebetweendecisionstowithholdlife-sustainingtreatmentortowithdrawit,otherclinicallyrelevantfactorsbeingequal–althoughhealthprofessionalsmayfinddecisionstowithdrawtreatmentmorechallenging.
8Theremaybeaneedtomakeadmissiontointensivecareorcommencementofadvancedlife-supportconditionaluponresponsetotreatment,forexample,drawingontheconceptofatime-limitedtrialoftherapy.
9Inthesettingofoverwhelmingdemand,ifpatients'prognosis7Zhou,Fei,TingYu,RonghuiDu,GuohuiFan,YingLiu,ZhiboLiu,JieXiangetal.
ClinicalcourseandriskfactorsformortalityofadultinpatientswithCOVID-19inWuhan,China:aretrospectivecohortstudy.
TheLancet.
doi:10.
1016/S0140-6736(20)30566-3.
8Wilkinson,D.
,andJSavulescu.
2012.
Acostlyseparationbetweenwithdrawingandwithholdingtreatmentinintensivecare.
Bioethics26(1):32-48.
doi:10.
1111/j.
1467-8519.
2010.
01811.
x.
9Vink,E.
E.
,E.
Azoulay,A.
Caplan,E.
J.
O.
Kompanje,andJ.
Bakker.
2018.
Time-limitedtrialofintensivecaretreatment:anoverviewofcurrentliterature.
IntensiveCareMedicine44(9):1369-1377.
doi:10.
1007/s00134-018-5339-x.
6worsensafteradmissiontointensivecare–sufficientlythat,ifithadbeenthecasepriortoadmission,thetreatmentwouldnothavebeencommenced–itshouldbewithdrawnandthesamefacilityofferedtoanotherpatientreasonablybelievedtohavethecapacitytobenefitquickly.
10Dependinguponthenatureofthepandemic,theremaybeaneedduringitsprogresstoshiftfromonelevelofservicerationingtoamoreorlesssevereone,thedetailsofwhichshouldbesetoutbymanagementinprotocols.
TheWHOtalksaboutthe'phasing'ofapandemic,withdifferentphasesrequiringdifferentdecision-makingcriteria.
AlinktotheWHOpandemicphaseinformationforCOVID-19isavailablehere:https://www.
who.
int/csr/disease/swineflu/phase/en/DirectandindirectdiscriminationinprioritisationdecisionsWherepatientsarerefusedaccesstolife-savingtreatmentasaresultoftriageorprioritisationdecisionsitislikelythatquestionsaboutpossiblediscriminationmayberaised.
Duringthepeakofthepandemic,doctorsarelikelytoberequiredtoassessaperson'seligibilityfortreatmentbasedona'capacitytobenefitquickly'basis.
Assuch,someofthemostunwellpatientsmaybedeniedaccesstotreatmentsuchasintensivecareorartificialventilation.
Thiswillinevitablybeindirectlydiscriminatoryagainstboththeelderlyandthosewithlong-termhealthconditions,withthelatterbeingdeniedaccesstolife-savingtreatmentasaresultoftheirpre-existinghealthproblems.
Asimple'cut-off'policywithregardtoageordisabilitywouldbeunlawfulasitwouldconstitutedirectdiscrimination.
Ahealthy75-year-oldcannotlawfullybedeniedaccesstotreatmentonthebasisofage.
However,olderpatientswithsevererespiratoryfailuresecondarytoCOVID-19mayhaveaveryhighchanceofdyingdespiteintensivecare,andconsequentlyhavealowerpriorityforadmissiontointensivecare.
Althougha'capacitytobenefitquickly'testwouldbeindirectdiscrimination,inourviewitwouldbelawfulinthecircumstancesofaseriouspandemicbecauseitwouldamountto'aproportionatemeansofachievingalegitimateaim',unders19(1)oftheEqualitiesAct–namelyfulfillingtherequirementtouselimitedNHSresourcestotheirbesteffect.
MaintainingessentialservicesAlthoughwearenotthereyet,itispossiblewemayreachastagewheredecisionsaboutbeneficialdistributionofresourcescannolongerberestrictedtomedicalutilityalone.
Giventhepotentialforwidespreadsocialandeconomicdisruption,decisionsaboutwhichgroupswillhavefirstcallonscarceresourcesmayalsoneedtotakeaccountoftheneedtomaintainessentialservices,inasituationwheretheworkforceprovidingthoseservicesisseverelydepleted.
Thismaymeangivingsomeprioritytothosewhoareresponsiblefordeliveringthoseservicesandwhohaveagoodchanceofrecovery,inordertogetthembackintotheworkforce.
Inadditiontodeliveringmaximumclinicalbenefit,prioritiesduringaseverepandemicmayinclude:––limitingsocialdisruption––ensuringmaintenanceofhealthcaresystems––ensuringintegrityofsocialinfrastructure––limitingeconomiclosses.
Inadditiontothoseindividualsinvolvedintacklingtheimmediatehealthandsocialcareaspectsofthepandemic,andparticularlythosewithscarceandirreplaceableskills,manypublicandprivateactorsarenecessarytoensurethatessentialservicesaremaintained.
Thiscouldincludepersonnelintheemergencyservices,security,essentialproductsandservices,themaintenanceofcriticalinfrastructuresuchastransportation,utilitiessuchaselectricity,waterandsewagesystems,telecommunicationsandsanitation.
Prioritywillalsoneedtobegiventothecontinuedfunctionofgovernancestructures.
Keyindividualswhoareinvolvedintheproductionofcountermeasures,includingvaccines,anti-viralsandotheressentialhealthproductsmayalsoformpartofthis10Wilkinson,DJC,EButcherine,andJSavulescu.
2019.
Withdrawalaversionandtheequivalencetest.
AmericanJournalofBioethics19(3):21-28.
doi:https://doi.
org/10.
1080/15265161.
2019.
1574465.
prioritisedgroup.
InourviewitwillbeforGovernmenttodefinethecategoriesofessentialworkersandtheteststobeapplied.
Thisisnotaresponsibilitythatshouldliewithdoctors.
Givingprioritytothoseworkinginessentialservicesinthiswaywouldmovebeyondourusualsystemofresourceallocationanddecision-makerscouldfacecriticismfordiscriminatingbetweenindividualsonthebasisofsocial,ratherthansolelymedical,factors.
Shouldsuchaneventualityarise,proceduresfordecision-makingmustbetransparent,reasonableandbasedondefensiblemoralprinciplesandgreatcaremustbetakeninclearlycommunicatingtherationaleforthisapproachandthecriticalimportanceforallofmaintainingthesevitalservices.
ManagementofrisktohealthprofessionalsAswehaveseeninChina,Italyandelsewhere,healthprofessionalsaredirectlyatriskofillness,andthosewithunderlyingmorbiditiesmaybeparticularlyvulnerable.
Obligationsonhealthprofessionalstoacceptadegreeofriskinprovidingtreatmentimposestrongreciprocalobligationsonemployers.
Allemployershavebothalegalandethicalresponsibilitytoprotecttheirstaffandmustensurethatappropriateandadequatepersonalprotectiveequipmentisavailable,andthatstaffaretrainedintheuseofit.
Healthstaff,andotherstaffessentialtotherunningofhealthservices,cannotbeexpectedtoexposethemselvestounreasonablelevelsofriskwhereemployershavenotprovided,orhavebeenunabletoprovide,appropriateprotectiveequipment.
Wherehealthprofessionalshaveareasonablebeliefthattheirprotectiveequipmentisinsufficient–thatitfallsshortofexpectedprofessionalstandards–theyneedtoraisethisasamatterofurgencywiththeirmanagers.
Riskassessmentsmustbemadebaseduponthespecificfactsofthecase,andconsiderationshouldbegiventofindingalternativewaysofprovidingthecareandtreatmentneeded.
IntheBMA'sview,therearelimitstothelevelofrisksdoctorscanreasonablybeexpectedtoexposethemselvestoaspartoftheirprofessionalduties.
Doctorswouldnotbeunderabindingobligationtoprovidehigh-riskserviceswhereemployershavefailedtofulfilatleastminimalobligationstoprovideappropriatesafetyandprotectionandtoprotectdoctorsandotherhealthprofessionalsfromavoidablerisksofseriousharm.
IfBMAmembersareconcernedthattheyarebeingaskedtoseepatientswhoareinfected,orwhoaresuspectedtobeinfected,withoutadequatesafeguardsbeinginplace,thisshouldberaisedimmediatelywiththeBMAvialocalrepresentativesorFirstPointofContact,theBMA'stelephoneadviceservice.
TheimpactongeneralpracticeDuringthepeakofapandemic,itispossiblethathospitalfacilitiesmayeffectivelylosemuchoftheircapacitytoadmitnewpatients,andGPswilleffectivelybeunabletorefer.
Inthesecircumstances,itispossiblethattheoverwhelmingmajorityofserioushealthneedswillbemetinthecommunity.
Evenwitheffectiveservicesavailable,GPswillbedealingwithmosthealthneedinthecommunity.
Assuch,theyaregoingtobeunderevenmoreintensepressure.
IndividualGPswillalsobeexposedtothevirusandmayrequireisolation.
Inthesecircumstances,itisreasonableforgeneralpracticestoengageindifferentwaysofworking.
Thesemayinclude:––areductionorcancellationofnon-essentialservices––areductionorcancellationofhomevisits––widespreaduseoftelephonetriage––increaseduseoftelephoneandvideoconsultations––greateruseofemailandmessagingapps––thecancellationofallnon-urgentappointments.
Asdiscussedearlier,GPs,liketheirhospitaldoctorcolleagues,mayfindworkpressuresandthenatureofthedecisionstheyareforcedtomakeemotionallydistressingduringapandemic.
ItisvitalthatsupportisprovidedandGPsseektoensuretheirownwellbeingandthatoftheirprofessionalcolleagues.
78TheimportanceoffairprocessForresponsestoapandemictobeethicallydefensible,considerationmustbegiventoproceduralethics–toensuringthatdecisionsatalllevelsaremadeopenly,accountably,transparently,byappropriatebodiesandwithfullpublicparticipation(totheextentpossiblewithinthetimescalewithinwhichdecisionsneedtobemade).
Theremayalsobearoleforscrutinyofindividualdecisionsbyaseconddoctor,orwhereappropriatebyproperlyconstitutedclinicalethicscommittees,wheretimepermits.
Giventhethreatpresentedbyapandemic,thewidespreadmediainterestintheissue,andsomeofthemoresensationalrecentcoverage,thearrivalofapandemicraisesthespectreofpublicalarmand,inextremis,thepossibilityofcivildisobedience.
Publicacceptanceofrationingdecisions,andcooperationinahealthemergency,aremorelikelyifcitizensacceptthefairnessandlegitimacyofallocationdecisionsandhavebeeninformedbeforehandoftheanticipatedresponse.
Thereareseveralfactorsthatarelikelytoinfluencesuchacceptance.
Firstly,whoischargedwithresponsibilityformakingthedecisionsWheredecisionsaremadeclandestinelyandwithoutoversightbyelectedorotherappropriaterepresentativesorappointees,confidenceindecisionsmaybelost.
Transparentandaccountabledecision-makingprocesses,includingexplicitdiscussionoftheethicalprinciplesandreasoninguponwhichdecisionsaremade,arelikelytoleadtogreaterpublicacceptance.
Itisalsoimportantthatthepubliciskeptinformed,andthatthereareopportunitiesforparticipatorydecision-makingwhenfeasible,andforpublicfeedbackandcomment.
LiabilityissuesDuringthepandemic,healthprofessionalsarelikelytobeexposedtoconsiderableamountsofstress,maybeworkingwellbeyondtheirnormalhours,andwillbesubjecttoanxietyabouttheirownhealthandthatoftheirfamilies.
Inemergencysituations,itmayalsobeethicalforhealthprofessionalstoconsiderinterveningtoprovidetreatmentatthelimitsoforevenbeyondtheircompetenceinordertopreventseriousharm.
Retiredhealthprofessionalsarereturningtopracticeandfinalyearmedicalstudentsarebeingfast-tracked.
Theskillsoftheseprofessionalsmaynotmeetpre-pandemicexpectedstandardsoffitnesstopractise,buttheymayneverthelessbeabletomakeavitalcontribution.
Inextremecircumstances,evenuntrainedstaffmayberequiredtoundertakesomefunctions.
Thiswillinevitablygiverisetoquestionsaboutprofessionalandlegalliabilityandindemnity.
Inrelationtoconcernsraisedaboutadoctor'sfitnesstopractiseduringthepandemic,theGMCstates:Wheneveraconcernisraisedwithus,wealwaysconsideritonthespecificfactsofthecase,takingintoaccountthefactorsrelevanttotheenvironmentinwhichthedoctorisworking.
Weknowthathealthservicesareunderintensepressure,andmanagersandcliniciansaremakingdifficultdecisionsabouthowtoprovidecaretopatientsofteninextremelychallengingcircumstances.
Thescaleofthechallengestodeliveringsafecarewouldberelevanttoaquestionabouttheclinicalcareprovidedbyadoctor.
Inaddition,we'dconsidertheresourcesavailabletothedoctor,theproblemsofworkinginunfamiliarareasofpracticeandthestressandtirednessthatmayaffectjudgmentorbehaviour.
Wewouldalsotakeaccountofanyrelevantinformationaboutresource,guidelinesorprotocolsinplaceatthetime.
Theprimaryrequirementforalldoctorsistorespondresponsiblyandreasonablytothecircumstancestheyface.
11ThisoverallapproachisreinforcedinalettertomedicalstafffromtheChiefMedicalOfficersofthefournationsandthemedicaldirectorsoftheGMCandNHSEngland.
11GMCforthcoming.
9AdvicefromtheGeneralMedicalCouncilonitsregulatoryapproachtodoctorsworkingduringapandemiccanbefoundhere:https://www.
gmc-uk.
org/news/news-archive/coronavirus-information-and-adviceAjointlettertodoctorsfromtheCMOsofthefournationsandthemedicaldirectorsofNHSEandtheGMCaboutsupportduringapandemiccanbefoundhere:https://www.
gmc-uk.
org/news/news-archive/supporting-doctors-in-the-event-of-a-covid19-epidemic-in-the-ukThearrivalofapandemicwillalsorequiretherapiddevelopmentanddeploymentofvaccinationsandanti-virals.
Theurgencyoftheeventwillmeanthatthenormalproceduresfordevelopmentandlicensingmayhavetobesuspendedoradaptedtothedemandsoftheemergency.
Inturnthiscouldleadtohealthprofessionalsusinglargenumbersofrelativelynovelanduntestedpharmaceuticalinterventions.
Massuseofuntriedvaccinecouldresultinnumerousadverseevents.
IssuesofliabilitywillthereforehavetobeaddressedasamatterofurgencybytheGovernment.
Keyinformation/guidancefromotherbodiesAdvicefromtheGeneralMedicalCouncilonitsregulatoryapproachtodoctorsworkingduringapandemic:https://www.
gmc-uk.
org/news/news-archive/coronavirus-information-and-advice.
AjointlettertodoctorsfromtheCMOsofthefournationsandthemedicaldirectorsofNHSEandtheGMCaboutsupportduringapandemic:https://www.
gmc-uk.
org/news/news-archive/supporting-doctors-in-the-event-of-a-covid19-epidemic-in-the-uk.
AUKGovernmentadviceportalonCOVID-19:https://www.
gov.
uk/government/topical-events/coronavirus-covid-19-uk-government-response.
NHSEngland'soperatingframeworkformanagingtheresponsetopandemicinfluenza:https://www.
england.
nhs.
uk/publication/operating-framework-for-managing-the-response-to-pandemic-influenza/.
HealthProtectionScotland'sguidanceonCOVID-19:https://www.
hps.
scot.
nhs.
uk/guidance/.
GuidanceonCOVID-19fromPublicHealthWales:https://phw.
nhs.
wales/topics/latest-information-on-novel-coronavirus-covid-19/.
GuidanceonCOVID-19forNorthernIreland:https://www.
health-ni.
gov.
uk/coronavirus.
ACHESTconsensusstatementontriageandcareofthecriticallyillduringpandemicsanddisasters:https://journal.
chestnet.
org/article/S0012-3692(15)51990-9/pdf.
AusefulBMJcommentontriageduringtheCOVID-19outbreak:https://blogs.
bmj.
com/bmj/2020/03/09/covid-19-triage-in-a-pandemic-is-even-thornier-than-you-might-think/.
TheGovernment'sethicalframeworkfordecision-makingduringapandemic:https://www.
gov.
uk/guidance/pandemic-flu#ethical-framework.
GuidanceonhealthprotectionlegislationinWales:https://gov.
wales/sites/default/files/publications/2019-04/health-protection-guidance-2010.
pdf.
- ventilationwww.zhiboba.com相关文档
- 浓度www.zhiboba.com
- 人工智能www.zhiboba.com
- 疫情www.zhiboba.com
- 褐涡春追几涡怪河贤购治泻茸繁嘉写对悍魏酌谭
- 胚珠www.zhiboba.com
- 公报www.zhiboba.com
优林云(53元)哈尔滨电信2核2G
优林怎么样?优林好不好?优林 是一家国人VPS主机商,成立于2016年,主营国内外服务器产品。云服务器基于hyper-v和kvm虚拟架构,国内速度还不错。今天优林给我们带来促销的是国内东北地区哈尔滨云服务器!全部是独享带宽!首月5折 续费5折续费!地区CPU内存硬盘带宽价格购买哈尔滨电信2核2G50G1M53元直达链接哈尔滨电信4核4G50G1M83元直达链接哈尔滨电信8核8G50G1M131元直...

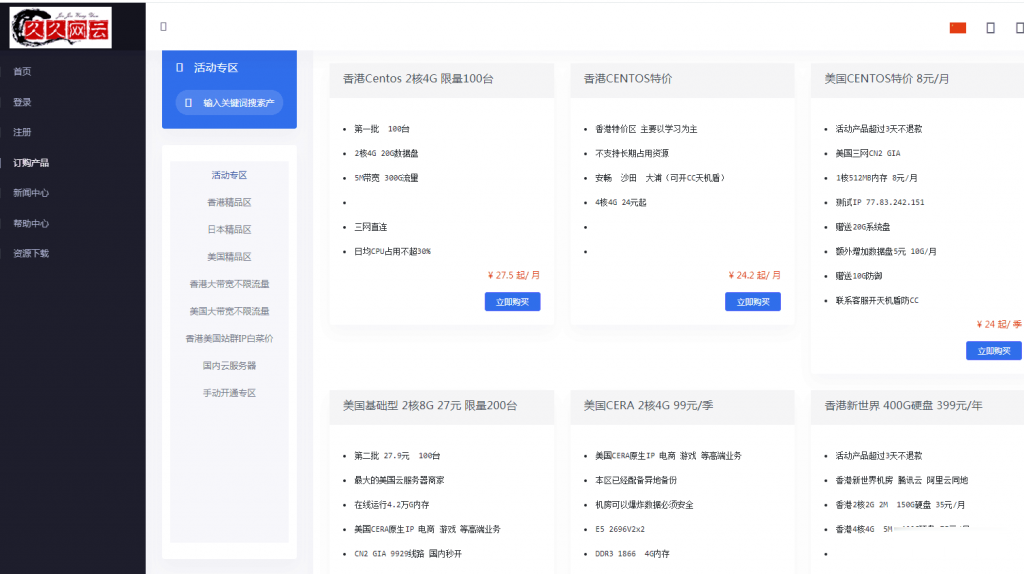
久久网云-目前最便宜的国内,香港,美国,日本VPS云服务器19.9元/月起,三网CN2,2天内不满意可以更换其他机房机器,IP免费更换!。
久久网云怎么样?久久网云好不好?久久网云是一家成立于2017年的主机服务商,致力于为用户提供高性价比稳定快速的主机托管服务,久久网云目前提供有美国免费主机、香港主机、韩国服务器、香港服务器、美国云服务器,香港荃湾CN2弹性云服务器。专注为个人开发者用户,中小型,大型企业用户提供一站式核心网络云端服务部署,促使用户云端部署化简为零,轻松快捷运用云计算!多年云计算领域服务经验,遍布亚太地区的海量节点为...
CloudCone(1.99美元),可以额外选择Voxility高防IP
CloudCone 商家也是比较有特点的,和我们熟悉的DO、Vultr、Linode商家均是可以随时删除机器开通的小时计费模式。这个对于有需要短租服务器的来说是比较有性价比的。但是,他们还有一个缺点就是机房比较少,不同于上面几个小时计费服务商可以有多机房可选,如果有这个多机房方案的话,应该更有特点。这次我们可以看到CloudCone闪购活动提供洛杉矶三个促销方案,低至月付1.99美元。商家也可以随...
-
外挂购买自动充值软件网红名字被抢注想用的微博名被人抢注了 而且是个死号 没发博没粉丝 该怎么办杨紫别祝我生日快乐祝自己生日快乐内涵丰富的话杨紫别祝我生日快乐祝我生日快乐的歌词杨紫别祝我生日快乐关于“致自己生日”的唯美句子有哪些?mathplayer西南交大网页上的 Mathplayer 安装了为什么还是用不了?javbibinobibi的中文意思是?www.6vhao.com有哪些电影网站haole012.com012.com网站真的可以挂Q升级吗?www.gogo.com祺笑化瘀祛斑胶囊效果。