D0www.236jj.com
www.236jj.com 时间:2021-04-06 阅读:()
RESEARCHOpenAccessPreventiveeffectofulinastatinonpostoperativecomplications,immunosuppression,andrecurrenceinesophagectomypatientsLingminZhang1,NingWang2,SunaZhou3,WenguangYe4,QinglinYao4,GuixiaJing1*andMingxinZhang4*AbstractBackground:Toevaluatethepotentialefficacyofpreventiveeffectofulinastatininesophagectomypatients.
Methods:Eightypatientswithesophagealcancerwerepreoperativelyallocatedatrandomintotwoequalgroups.
Ulinastatinwasadministeredtothetreatmentgroup(U)whereasthecontrolgroup(C)receivedaplacebo.
Thearterialoxygentensionandcarbondioxidetensionweremeasuredandtherespiratoryindex(RI)wascalculated.
PlasmalevelsofcirculatingTlymphocytesubsetsandinterleukin6(IL-6)weremeasuredandclinicalcoursesofpatientsinthetwogroupswerecompared.
Results:RIintheUgroupwassignificantlylowerthanthatintheCgroup.
TherateofpostoperativecomplicationsandthedurationofICUstayweresignificantlylowerintheUgroup.
UlinastatinsignificantlyincreasedtherateofCD3+andCD4+cells,andratioofCD4+/CD8+,butdecreasedtherateofCD8+cellsandreleaseofIL-6comparedtotheCgrouponpostoperativedays1and3.
PatientswithintheCgroupshowedworserecurrencefreesurvival.
Multivariateanalysisrevealedthatulinastatinadministrationsignificantlydecreasedtheincidenceofrecurrence.
Conclusions:Ulinastatinhadapreventiveeffectonpostoperativecomplicationsandimmunosuppressioninesophagectomypatients,therebyprolongingrecurrencefreesurvival.
Keywords:Esophagectomy,Immunosuppression,Postoperativecomplications,Recurrence,UlinastatinBackgroundSurgeryremainsthemosteffectivetreatmentforsolidtumorsincludingesophagealcancer.
However,esopha-gectomy,oneofthemostinvasiveproceduresamonggastrointestinaloperations,hasahighfrequencyofpost-operativecomplications[1].
Severalresponsibleback-groundfactorshavebeenproposedtoexplainthebroadspectrumofpostoperativecomplicationsaftersuchin-vasiveprocedures.
Themostimportantonesaresyste-micinflammatoryresponsesyndromeandcompensatoryanti-inflammatorycytokineresponsesyndrome[2-4].
Moreover,surgicalstresscancauseimmunosuppres-sioninresponsetothecomplexinteractionofvarioushormones,cytokines,andacutephasereactants[5].
Ithasbeenreportedthatperioperativeandpostoperativeimmunosuppressionincreasestheratioofrecurrenceandadverselyaffectstheprognosisofcancerpatients[6,7].
Therefore,itisdesirabletofindaneffectivecountermeasureagainsttheoverproductionofproin-flammatorycytokines,postoperativecomplications,andimmunosuppression.
Ulinastatinisaserineproteaseinhibitorwithamo-lecularweightof~67,000foundinhealthyhumanurine.
Itisusedworldwideforpatientswithinflammatorydis-orders,includingdisseminatedintravascularcoagulation,shock,andpancreatitis[8-10].
Furthermore,ulinastatinadministrationcanhelpreducethesurgicalstress,pre-ventradiation-inducedlunginjury,andmodulateim-munefunctions[11-13].
Theaimofthepresentstudywastoevaluatethepotentialefficacyofpreventiveeffectofulinastatinon*Correspondence:jgx666@126.
com;zmx3115@163.
comEqualcontributors1DepartmentofAnesthesiology,FirstAffiliatedHospital,MedicalSchool,Xi'anJiaotongUniversity,Xi'an710061,ShaanxiProvince,China4DepartmentofGastroenterology,TangduHospital,FourthMilitaryMedicalUniversity,Xi'an710038,ShaanxiProvince,ChinaFulllistofauthorinformationisavailableattheendofthearticleWORLDJOURNALOFSURGICALONCOLOGY2013Zhangetal.
;licenseeBioMedCentralLtd.
ThisisanOpenAccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/2.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84http://www.
wjso.
com/content/11/1/84postoperativecomplications,immunosuppression,andrecurrenceinesophagectomypatients.
MethodsPatientsBetweenJanuary2007andDecember2007,patientswithlowerthoracicesophagealcancerrequiringsurgicalin-terventionattheFirstAffiliatedHospitalandSecondAffiliatedHospital,MedicalCollegeofXi'anJiaotongUniversity,wereenrolled.
Exclusioncriteria:priorche-motherapyorirradiationorimmunosuppressivedrugadministration;bloodloss≥1,000mL;ASAclassifica-tion≥III,histologicaltypeofadenocarcinoma.
Eightypatientsweresubsequentlyrandomizedintotwogroups:controlgroup(C,n=40)andulinastatingroup(U,n=40).
Theoperativeprocedureforremovalofthecancerwasperformedbyasinglesurgicalteamandthroughtheleftposterolateralthoracotomyapproachwithcombinedtho-racoabdominallymphaticdissection,proximalgastricre-sectionandmobilizationofthestomachforesophagealreplacement.
InstitutionalEthicsCommitteeapprovalforthisprojectwasobtained.
Writteninformedconsentwasobtainedfromeachpatientbeforerandomization.
Thestudywasdesignedasasingleblindedstudy.
Ulinastatin(Miraclid,MochidaPharmaceulinastatincal,Japan)wasadministeredtotheUgroupasabolusof200,000Udilutedin20mLofnormalsalineevery24hfrom3dayspre-operationuntil3dayspost-operation.
ClinicalcourseevaluationClinicalcoursewasevaluatedbasedonrateofpostope-rativecomplications,includingcardiovascularcomplica-tions(arrhythmia,pulmonaryembolism,andmyocardialinfarction),pulmonarycomplications(pneumonia,ate-lectasis,pulmonaryedema),andothers(esophagogastricanastomosisleakage,stenosis,andwoundinfection).
Thecriteriaofpostoperativecomplications,especiallyforpul-monarycomplications,weredescribedasbefore[14].
ThedurationofICUandhospitalstaywasalsodetermined.
Allpatientsreceivedcisplatin-basedpostoperativead-juvantchemotherapyorstandardradiotherapy,ifrequired.
Thefollow-upperiodrangedfrom1to48months(median,35.
7months).
Computedtomography(CT)wasperformedatleastevery6monthstodetectrecurrence.
SamplecollectionandassayArterialbloodwascollectedimmediatelyat10minutesafteroperationbegan(T1),1hourafterone-lungventila-tion(T2),andatthetimeofclosure(T3).
Arterialoxygentension(PaO2)andcarbondioxidetension(PaCO2)weremeasuredbybloodgasanalysis.
Therespiratoryindex(RI)wascalculatedasamarkeroflungdamageusingthefollowingformulas:RI=[FIO2*(760–47)-PaCO2/0.
8]/PaO2.
Peripheralwholebloodsampleswereobtained1hourbeforesurgery(D0)andonpostoperativedays1,3,and7(D1,D2,andD3).
LymphocytesubsetswerecountedbyaFACSCalibur(BectonDickinson,SanJose,CA,USA)flowcytometer.
Cytokinelevels(IL-6)weredeterminedbyELISA,usingcommerciallyavailablekits(R&DSystems,Minneapolis,MN,USA).
StatisticsDataareexpressedasmean±standarddeviation.
Sta-tisticalanalysiswasperformedwiththeSPSSsoftwarepackage(version13.
0,SPSSInstitute).
Continuousvari-ableswereanalyzedusingrepeatedmeasuresANOVAandcategoricaldatawerecomparedbytheχ2testorFisher'sexacttest.
SurvivalcurveswereestimatedbytheKaplan-Meiermethodwiththelog-ranktest.
Multivari-ateanalysiswasperformedusingtheCoxproportionalhazardregressionanalysis.
Pvalues<0.
05wereconsi-deredsignificant.
Table1Baselinecharacteristicsofthe80patientsControl(n=40)Ulinastatin(n=40)PAge56±1256±100.
861Gender(male/female)34/633/70.
762TNMstage(I/II/III)7/18/156/20/140.
897Lengthofresection(cm)10±4.
811±4.
00.
157Numberoflymphnodedissection11±4.
110±4.
60.
154Alcoholconsumption(yes/no)25/1523/170.
648Smoker(yes/no)21/1920/200.
823FEV1/FVC(%)85.
3±3.
385.
1±4.
30.
769ASAclassification(I/II)18/2217/230.
822Durationofoperation(min)206±44207±430.
918Durationofanesthesia(min)240±46242±440.
862Bloodlossduringoperation(mL)520±43518±620.
903Figure1Effectofulinastatinonrespiratoryindex.
Respiratoryindex(RI)intheulinastatingroup(U)wassignificantlylowerthanthatinthecontrolgroup(C)1hourafterone-lungventilation(T2)andthetimeofsternalclosure(T3;P<0.
05).
TheRIwascalculatedasamarkeroflungdamageusingthefollowingformulas:RI=[FIO2*(760–47)-PaCO2/0.
8]/PaO2.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page2of6http://www.
wjso.
com/content/11/1/84ResultsBaselinecharacteristicsofenrolledpatientsDuringaperiodof12monthsbetweenJanuary2007andDecember2007,80patientsundergoingesophagecto-mywereenrolledinthisstudy.
BackgroundfactorsforesophagealcancerpatientsarelistedinTable1.
Therewerenosignificantdifferencesbetweenthegroupsinaverageage,gender,TNMstage,lengthofresection,numberoflymphnodedissection,alcoholconsumption,smoking,ASAclassification,durationofoperation,dur-ationofanesthesia,andbloodlossduringoperation.
Typeofanesthesiawasthesamebetweenthetwogroups.
Therewerealsonosignificantdifferencesinperi-operativemanagement,includingtheusageofsteroidandelastaseinhibitor,infusionandnutritionalsupport,andNSAIDsandotheranalgesics,betweenthetwogroups.
EffectofulinastatinonrespiratoryindexRIbeforeoperationdidnotdiffersignificantlybetweenthegroups(groupUvs.
C,0.
29±0.
07vs.
0.
31±0.
06),andthereweresignificanttime-dependentchangesinRIvalueinbothgroups(P<0.
05,Figure1).
GroupUsho-wedsignificantlylowerRIvaluesthanthatofgroupC,bothat1hourafterone-lungventilation(T2)(0.
40±0.
09Table2EffectofulinastatinonpostoperativeclinicalcourseControl(n=40)Ulinastatin(n=40)PCardiovascularcomplications111Pulmonarycomplications810.
034Anastomosisleakage111Anastomosisstenosis101Woundinfection111Total1240.
034Death101DurationofICUstay(hours)45±2433±160.
01Lengthofhospitalstay(days)11±410±20.
170Figure2EffectofulinastatinonlymphocytesubsetsandIL-6.
Ulinastatin(U)administrationsignificantlyincreasedtherateofCD3+(A)andCD4+(B)cells,andratioofCD4+/CD8+(D),butdecreasedtherateofCD8+(C)cellsandreleaseofIL-6(E)comparedtocontrolgroup(C)onpostoperativedays1(D1)and3(D2;P<0.
05).
D0=1hourbeforesurgery,D3=Postoperativeday7.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page3of6http://www.
wjso.
com/content/11/1/84vs.
0.
53±0.
11,P<0.
05)andthetimeofsternalclosure(T3)(0.
75±0.
16vs.
0.
90±0.
17,P<0.
05).
EffectofulinastatinonpostoperativeclinicalcourseThepostoperativeclinicalcourseofeachpatientwascare-fullymonitoreddaily,andcomplicationswerechecked(Table2).
Postoperativecomplicationswereobservedin12patients(30%)intheCgroupand4patients(10%)intheUgroup,respectively(P<0.
05).
AsignificantdecreaseinpulmonarycomplicationswasobservedintheUgroup(P<0.
05),andonepatientintheCgroupdiedofpul-monaryoedema.
Althoughlengthofhospitalstayshowednosignificantdifferencesbetweenthetwogroups,thedurationofICUstaywassignificantlyshorterintheUgroup(P<0.
05).
AscanbeseenfromFigure2,ulinastatinadministra-tionsignificantlyincreasedtherateofCD3+andCD4+cells,andratioofCD4+/CD8+,butdecreasedtherateofCD8+cellsandreleaseofIL-6comparedtotheCgrouponD1andD2(P<0.
05).
SideeffectsNopatientexperiencedsideeffectsrelatedtoulinastatinadministration;namely,shock,itching,rash,nausea,vo-miting,orneutropenia.
SurvivalanalysisOf80patientsinthedatabase,onepatientdiedintheCgroupduringtheperioperativeperiod,and3werelosttofollow-up.
Asaresult,76patientswereenrolledforsurvivalanalysis.
TherecurrencerateoftheUgroupwas57.
5%comparedto72.
5%intheCgroup.
Themostcommonrecurrencepatternwaslocoregionalrecurrence(60%intheUgroupand72%intheCgroup),whileotherpatientsdevelopedsystemicrecurrenceoracom-binationofboth.
Recurrence-freesurvivalofallpatientswas33.
8±1.
7months,anditwasstatisticallybetterfortheUgroup(39.
4±2.
2)comparedtotheCgroup(27.
8±2.
4)byKaplan-Meieranalysis(P<0.
05,Figure3).
Multivariateanalysisrevealedthatulinastatinadminis-trationsignificantlydecreasedtheincidenceofrecur-rence(Table3).
DiscussionMajorstressfulsurgeryincludingesophagectomyalwayscausedoverproductionofproinflammatorycytokines.
Theinitialproinflammatoryresponsemaybeuncon-trolledcausinganimbalancebetweeninflammatoryre-sponsesyndromeandcompensatoryanti-inflammatorycytokineresponsesyndrome,whichledtopostoperativecomplications[15].
Forthespecialsurgicalprocedures,theriskofpulmonarycomplicationsafteresophagec-tomyishigherthananyothercommonoperation[16].
Moreover,surgicalstresscancauseimmunosuppressionFigure3Kaplan-Meiersurvivalanalysis.
CumulativerecurrencefreesurvivaldifferencesbetweenpatientsintheCandUgroups.
PatientswithintheCgroupshowedworserecurrencefreesurvival.
Pvaluewasobtainedusingthelog-ranktestofthedifference.
Table3MultivariatecoxproportionalhazardsanalysisforrecurrencefreesurvivalVariablesRecurrencefreesurvivalPRR95%CIUlinastatinadministration0.
1490.
063-0.
351<0.
05TNM1.
8120.
652-5.
0380.
254Alcoholconsumption2.
0660.
909-4.
3440.
757Smoking1.
0880.
534-2.
2170.
817Gender0.
9160.
425-1.
9730.
822Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page4of6http://www.
wjso.
com/content/11/1/84inresponsetooverproductionofproinflammatorycytoki-nes.
Inesophagealcancer,aprognosticrelationbetweenthepresenceofcomplicationsandimmunosuppressionafteresophagectomyandsurvivalhaspreviouslybeenreported[17,18].
Thesedatasuggestthataneffectivecountermeasureagainstpostoperativecomplicationsandimmunosuppressionisdesirable.
Ulinastatinhasmanyphysiologicaleffectsinsurgicalstress,includingthedecreaseoftheinflammatoryre-action,inhibitionofimmunosuppression,andmodifica-tionofthewaterbalance[13,19,20].
Moreover,previousstudieshaveshownthatulinastatininhibitshumanovar-iancancerandtheeffectcouldberelatedtodown-regulationofproteinkinaseC[21].
Studieshavealsofoundthatulinastatinenhancestheinhibitoryeffectofdocetaxelinbreastcancerbyamechanismconsistentwiththedown-regulatedexpressionofIL-6,IL-8,andTNF-α[22].
Sinceulinastatinhadapreventiveeffectonpostoperativecomplicationsandimmunosuppression,andmightinhibitthegrowthofcancercells,wechoseitforthecertainpurpose.
CD3+,CD4+,CD8+T-lymphocytepercentageandCD4+/CD8+ratiowerecloselyrelatedtothecellularim-munefunctionandpostoperativeanti-tumorimmunity[23-25].
Moreover,lowerCD3+,lowerCD4+andlowerCD4+/CD8+ratiowerefactorsindependentlyassociatedwithworseprognosisofesophagealcancerpatientsindifferentreports[26,27].
Therefore,weinvestigatedef-fectofulinastatinadministrationoncontentoflympho-cytesubsets.
Inthepresentstudy,itwasfoundthatulinastatinad-ministrationhadaprotectiveeffectonpulmonaryfunc-tionbydecreasingtheincreasingtrendofRIduringoperation.
Asaresult,thepostoperativecomplicationswerelowerthanthatintheCgroup,especiallyforpul-monarycomplications.
LowoccurrenceofpostoperativecomplicationsshortensthedurationofICUstayandde-creasedcostofcare.
Further,weinvestigatedtheeffectofulinastatinonreleaseofIL-6andcontentoflym-phocytesubsets.
Thechangeofpost-operativeIL-6andlymphocytesubsetsreflectedbeneficialeffectsofuli-nastatinonanti-inflammatoryaction,postoperativeim-munosuppression,andpostoperativeanti-tumorresponse.
Finally,weobservedthattheUgrouphadalongerrecur-rencefreesurvival.
ConclusionsFromtheseresultsweconcludedthatulinastatinhadapreventiveeffectonpostoperativecomplicationsandimmunosuppressioninesophagectomypatients,thereby,prolongingrecurrencefreesurvival.
Thepossiblereasonmaybethattheenhancedanti-tumorresponseinhibitedtumormetastasis[28,29].
However,thedetailedmecha-nismofactionofulinastatinshouldbefurtherstudiedatthemolecularbiologicallevel.
Evaluationofalargenum-berofcasesisalsonecessarytoassesstheclinicaluseful-nessofulinastatin.
AbbreviationsIL-6:Interleukin-6;RI:Respiratoryindex.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Authors'contributionsLMandNWparticipatedinthedesignandconductionofexperiments,dataanalysis,andfinaldraftingandwritingofthemanuscript.
LM,NW,SZandWYallcontributedtotheseexperiments.
GJandMZwerecloselyinvolvedinresearchdesignanddraftingofthefinalmanuscript.
Allauthorsreadandapprovedthefinalmanuscript.
Authordetails1DepartmentofAnesthesiology,FirstAffiliatedHospital,MedicalSchool,Xi'anJiaotongUniversity,Xi'an710061,ShaanxiProvince,China.
2DepartmentofAnesthesiology,SecondAffiliatedHospital,MedicalSchool,Xi'anJiaotongUniversity,Xi'an710061,ShaanxiProvince,China.
3DepartmentofRadiotherapy,TangduHospital,FourthMilitaryMedicalUniversity,Xi'an710038,ShaanxiProvince,China.
4DepartmentofGastroenterology,TangduHospital,FourthMilitaryMedicalUniversity,Xi'an710038,ShaanxiProvince,China.
Received:28October2012Accepted:26March2013Published:10April2013References1.
WhooleyBP,LawS,MurthySC,AlexandrouA,WongJ:Analysisofreduceddeathandcomplicationratesafteresophagealresection.
AnnSurg2001,233:338–344.
2.
SatoN,KoedaK,IkedaK,KimuraY,AokiK,IwayaT,AkiyamaY,IshidaK,SaitoK,EndoS:Randomizedstudyofthebenefitsofpreoperativecorticosteroidadministrationonthepostoperativemorbidityandcytokineresponseinpatientsundergoingsurgeryforesophagealcancer.
AnnSurg2002,236:184–190.
3.
SudaK,KitagawaY,OzawaS,SaikawaY,UedaM,AbrahamE,KitajimaM,IshizakaA:Serumconcentrationsofhigh-mobilitygroupboxchromosomalprotein1beforeandafterexposuretothesurgicalstressofthoracicesophagectomy:apredictorofclinicalcourseaftersurgeryDisEsophagus2006,19:5–9.
4.
YamaguchiY,HiharaJ,HironakaK,OhshitaA,OkitaR,OkawakiM,MatsuuraK,NagamineI,IkedaT,OharaM,HamaiY:Postoperativeimmunosuppressioncascadeandimmunotherapyusinglymphokine-activatedkillercellsforpatientswithesophagealcancer:possibleapplicationforcompensatoryanti-inflammatoryresponsesyndrome.
OncolRep2006,15:895–901.
5.
KhansariDN,MurgoAJ,FaithRE:Effectsofstressontheimmunesystem.
ImmunolToday1990,11:170–175.
6.
OgawaK,HiraiM,KatsubeT,MurayamaM,HamaguchiK,ShimakawaT,NaritakeY,HosokawaT,KajiwaraT:Suppressionofcellularimmunitybysurgicalstress.
Surgery2000,127:329–336.
7.
ShakharG,Ben-EliyahuS:Potentialprophylacticmeasuresagainstpostoperativeimmunosuppression:couldtheyreducerecurrenceratesinoncologicalpatientsAnnSurgOncol2003,10:972–992.
8.
MasudaT,SatoK,NodaC,IkedaKM,MatsunagaA,OguraMN,ShimizuK,NagasawaH,MatsuyamaN,IzumiT:Protectiveeffectofurinarytrypsininhibitoronmyocardialmitochondriaduringhemorrhagicshockandreperfusion.
CritCareMed2003,31:1987–1992.
9.
InoueK,TakanoH,YanagisawaR,YoshikawaT:Protectiveeffectsofurinarytrypsininhibitoronsystemicinflammatoryresponseinducedbylipopolysaccharide.
JClinBiochemNutr2008,43:139–142.
10.
UemuraK,MurakamiY,HayashidaniY,SudoT,HashimotoY,OhgeH,SuedaT:Randomizedclinicaltrialtoassesstheefficacyofulinastatinforpostoperativepancreatitisfollowingpancreaticoduodenectomy.
JSurgOncol2008,98:309–313.
11.
OnoS,AosasaS,MochizukiH:Effectsofaproteaseinhibitoronreductionofsurgicalstressinesophagectomy.
AmJSurg1999,177:78–82.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page5of6http://www.
wjso.
com/content/11/1/8412.
BaoP,GaoW,LiS,ZhangL,QuS,WuC,QiH:Effectofpretreatmentwithhigh-doseulinastatininpreventingradiation-inducedpulmonaryinjuryinrats.
EurJPharmacol2009,603:114–119.
13.
SatoN,EndoS,KimuraY,IkedaK,AokiK,IwayaT,AkiyamaY,NodaY,SaitoK:Influenceofahumanproteaseinhibitoronsurgicalstressinducedimmunosuppression.
DigSurg2002,19:300–305.
14.
D'JournoXB,MicheletP,MarinV,DiesnisI,BlayacD,DoddoliC,BongrandP,ThomasPA:Anearlyinflammatoryresponsetooesophagectomypredictstheoccurrenceofpulmonarycomplications.
EurJCardiothoracSurg2010,37:1144–1151.
15.
LinE,LowrySF:Inflammatorycytokinesinmajorsurgery:afunctionalperspective.
IntensiveCareMed1999,25:255–257.
16.
FergusonMK,DurkinAE:Preoperativepredictionoftheriskofpulmonarycomplicationsafteresophagectomyforcancer.
JThoracCardiovascSurg2002,123:661–669.
17.
LagardeSM,deBoerJD,tenKateFJ,BuschOR,ObertopH,vanLanschotJJ:Postoperativecomplicationsafteresophagectomyforadenocarcinomaoftheesophagusarerelatedtotimingofdeathduetorecurrence.
AnnSurg2008,247:71–76.
18.
TakagiK,YamamoriH,MorishimaY,ToyodaY,NakajimaN,TashiroT:Preoperativeimmunosuppression:itsrelationshipwithhighmorbidityandmortalityinpatientsreceivingthoracicesophagectomy.
Nutrition2001,17:13–17.
19.
ParkJH,KwakSH,JeongCW,BaeHB,KimSJ:Effectofulinastatinoncytokinereactionduringgastrectomy.
KoreanJAnesthesiol2010,58:334–337.
20.
SatoA,KuwabaraY,ShinodaN,KimuraM,IshiguroH,FujiiY:Useoflowdosedopamine,gabexatemesilateandulinastatinreducesthewaterbalanceandpulmonarycomplicationinthoracicesophagectomypatients.
DisEsophagus2005,18:151–154.
21.
KobayashiH,SuzukiM,TanakaY,HirashimaY,TeraoT:SuppressionofurokinaseexpressionandinvasivenessbyurinarytrypsininhibitorismediatedthroughinhibitionofproteinkinaseC-andMEK/ERK/c-Jun-dependentsignalingpathways.
JBiolChem2001,276:2015–2022.
22.
ZhaoX,SunX,GaoF,LuoJ,SunZ:EffectsofulinastatinanddocetaxelonbreasttumorgrowthandexpressionofIL-6,IL-8,andTNF-α.
JExpClinCancerRes2011,30:22.
23.
UchidaK,KusudaT,KoyabuM,MiyoshiH,FukataN,SumimotoK,FukuiY,SakaguchiY,IkeuraT,ShimataniM:RegulatoryTcellsintype1autoimmunepancreatitis.
IntJRheumatol2012,2012:795026.
24.
YuWK,LiWQ,LiN,LiJS:Mononuclearhistocompatibilityleukocyteantigen-DRexpressionintheearlyphaseofacutepancreatitis.
Pancreatology2004,4:233–243.
25.
ChenL,LinsleyPS,HellstrmKE:CostimulationofTcellsfortumorimmunity.
ImmunolToday1993,14:483–486.
26.
NozoeT,MaeharaY,SugimachiK:PreoperativesortingofcirculatingTlymphocytesinpatientswithesophagealsquamouscellcarcinoma:itsprognosticsignificance.
WorldJGastroenterol2005,11:6689–6693.
27.
GuoSJ,LinDM,LiJ,LiuRZ,ZhouCX,WangDM,MaWB,ZhangYH,ZhangSR:Tumor-associatedmacrophagesandCD3-zetaexpressionoftumor-infiltratinglymphocytesinhumanesophagealsquamous-cellcarcinoma.
DisEsophagus2007,20:107–116.
28.
SheuBC,HsuSM,HoHN,LinRH,TorngPL,HuangSC:ReversedCD4/CD8ratiosoftumor-infiltratinglymphocytesarecorrelatedwiththeprogressionofhumancervicalcarcinoma.
Cancer1999,86:1537–1543.
29.
BalkwillF:Cancerandthechemokinenetwork.
NatRevCancer2004,4:540–550.
doi:10.
1186/1477-7819-11-84Citethisarticleas:Zhangetal.
:Preventiveeffectofulinastatinonpostoperativecomplications,immunosuppression,andrecurrenceinesophagectomypatients.
WorldJournalofSurgicalOncology201311:84.
SubmityournextmanuscripttoBioMedCentralandtakefulladvantageof:ConvenientonlinesubmissionThoroughpeerreviewNospaceconstraintsorcolorgurechargesImmediatepublicationonacceptanceInclusioninPubMed,CAS,ScopusandGoogleScholarResearchwhichisfreelyavailableforredistributionSubmityourmanuscriptatwww.
biomedcentral.
com/submitZhangetal.
WorldJournalofSurgicalOncology2013,11:84Page6of6http://www.
wjso.
com/content/11/1/84
Methods:Eightypatientswithesophagealcancerwerepreoperativelyallocatedatrandomintotwoequalgroups.
Ulinastatinwasadministeredtothetreatmentgroup(U)whereasthecontrolgroup(C)receivedaplacebo.
Thearterialoxygentensionandcarbondioxidetensionweremeasuredandtherespiratoryindex(RI)wascalculated.
PlasmalevelsofcirculatingTlymphocytesubsetsandinterleukin6(IL-6)weremeasuredandclinicalcoursesofpatientsinthetwogroupswerecompared.
Results:RIintheUgroupwassignificantlylowerthanthatintheCgroup.
TherateofpostoperativecomplicationsandthedurationofICUstayweresignificantlylowerintheUgroup.
UlinastatinsignificantlyincreasedtherateofCD3+andCD4+cells,andratioofCD4+/CD8+,butdecreasedtherateofCD8+cellsandreleaseofIL-6comparedtotheCgrouponpostoperativedays1and3.
PatientswithintheCgroupshowedworserecurrencefreesurvival.
Multivariateanalysisrevealedthatulinastatinadministrationsignificantlydecreasedtheincidenceofrecurrence.
Conclusions:Ulinastatinhadapreventiveeffectonpostoperativecomplicationsandimmunosuppressioninesophagectomypatients,therebyprolongingrecurrencefreesurvival.
Keywords:Esophagectomy,Immunosuppression,Postoperativecomplications,Recurrence,UlinastatinBackgroundSurgeryremainsthemosteffectivetreatmentforsolidtumorsincludingesophagealcancer.
However,esopha-gectomy,oneofthemostinvasiveproceduresamonggastrointestinaloperations,hasahighfrequencyofpost-operativecomplications[1].
Severalresponsibleback-groundfactorshavebeenproposedtoexplainthebroadspectrumofpostoperativecomplicationsaftersuchin-vasiveprocedures.
Themostimportantonesaresyste-micinflammatoryresponsesyndromeandcompensatoryanti-inflammatorycytokineresponsesyndrome[2-4].
Moreover,surgicalstresscancauseimmunosuppres-sioninresponsetothecomplexinteractionofvarioushormones,cytokines,andacutephasereactants[5].
Ithasbeenreportedthatperioperativeandpostoperativeimmunosuppressionincreasestheratioofrecurrenceandadverselyaffectstheprognosisofcancerpatients[6,7].
Therefore,itisdesirabletofindaneffectivecountermeasureagainsttheoverproductionofproin-flammatorycytokines,postoperativecomplications,andimmunosuppression.
Ulinastatinisaserineproteaseinhibitorwithamo-lecularweightof~67,000foundinhealthyhumanurine.
Itisusedworldwideforpatientswithinflammatorydis-orders,includingdisseminatedintravascularcoagulation,shock,andpancreatitis[8-10].
Furthermore,ulinastatinadministrationcanhelpreducethesurgicalstress,pre-ventradiation-inducedlunginjury,andmodulateim-munefunctions[11-13].
Theaimofthepresentstudywastoevaluatethepotentialefficacyofpreventiveeffectofulinastatinon*Correspondence:jgx666@126.
com;zmx3115@163.
comEqualcontributors1DepartmentofAnesthesiology,FirstAffiliatedHospital,MedicalSchool,Xi'anJiaotongUniversity,Xi'an710061,ShaanxiProvince,China4DepartmentofGastroenterology,TangduHospital,FourthMilitaryMedicalUniversity,Xi'an710038,ShaanxiProvince,ChinaFulllistofauthorinformationisavailableattheendofthearticleWORLDJOURNALOFSURGICALONCOLOGY2013Zhangetal.
;licenseeBioMedCentralLtd.
ThisisanOpenAccessarticledistributedunderthetermsoftheCreativeCommonsAttributionLicense(http://creativecommons.
org/licenses/by/2.
0),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedtheoriginalworkisproperlycited.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84http://www.
wjso.
com/content/11/1/84postoperativecomplications,immunosuppression,andrecurrenceinesophagectomypatients.
MethodsPatientsBetweenJanuary2007andDecember2007,patientswithlowerthoracicesophagealcancerrequiringsurgicalin-terventionattheFirstAffiliatedHospitalandSecondAffiliatedHospital,MedicalCollegeofXi'anJiaotongUniversity,wereenrolled.
Exclusioncriteria:priorche-motherapyorirradiationorimmunosuppressivedrugadministration;bloodloss≥1,000mL;ASAclassifica-tion≥III,histologicaltypeofadenocarcinoma.
Eightypatientsweresubsequentlyrandomizedintotwogroups:controlgroup(C,n=40)andulinastatingroup(U,n=40).
Theoperativeprocedureforremovalofthecancerwasperformedbyasinglesurgicalteamandthroughtheleftposterolateralthoracotomyapproachwithcombinedtho-racoabdominallymphaticdissection,proximalgastricre-sectionandmobilizationofthestomachforesophagealreplacement.
InstitutionalEthicsCommitteeapprovalforthisprojectwasobtained.
Writteninformedconsentwasobtainedfromeachpatientbeforerandomization.
Thestudywasdesignedasasingleblindedstudy.
Ulinastatin(Miraclid,MochidaPharmaceulinastatincal,Japan)wasadministeredtotheUgroupasabolusof200,000Udilutedin20mLofnormalsalineevery24hfrom3dayspre-operationuntil3dayspost-operation.
ClinicalcourseevaluationClinicalcoursewasevaluatedbasedonrateofpostope-rativecomplications,includingcardiovascularcomplica-tions(arrhythmia,pulmonaryembolism,andmyocardialinfarction),pulmonarycomplications(pneumonia,ate-lectasis,pulmonaryedema),andothers(esophagogastricanastomosisleakage,stenosis,andwoundinfection).
Thecriteriaofpostoperativecomplications,especiallyforpul-monarycomplications,weredescribedasbefore[14].
ThedurationofICUandhospitalstaywasalsodetermined.
Allpatientsreceivedcisplatin-basedpostoperativead-juvantchemotherapyorstandardradiotherapy,ifrequired.
Thefollow-upperiodrangedfrom1to48months(median,35.
7months).
Computedtomography(CT)wasperformedatleastevery6monthstodetectrecurrence.
SamplecollectionandassayArterialbloodwascollectedimmediatelyat10minutesafteroperationbegan(T1),1hourafterone-lungventila-tion(T2),andatthetimeofclosure(T3).
Arterialoxygentension(PaO2)andcarbondioxidetension(PaCO2)weremeasuredbybloodgasanalysis.
Therespiratoryindex(RI)wascalculatedasamarkeroflungdamageusingthefollowingformulas:RI=[FIO2*(760–47)-PaCO2/0.
8]/PaO2.
Peripheralwholebloodsampleswereobtained1hourbeforesurgery(D0)andonpostoperativedays1,3,and7(D1,D2,andD3).
LymphocytesubsetswerecountedbyaFACSCalibur(BectonDickinson,SanJose,CA,USA)flowcytometer.
Cytokinelevels(IL-6)weredeterminedbyELISA,usingcommerciallyavailablekits(R&DSystems,Minneapolis,MN,USA).
StatisticsDataareexpressedasmean±standarddeviation.
Sta-tisticalanalysiswasperformedwiththeSPSSsoftwarepackage(version13.
0,SPSSInstitute).
Continuousvari-ableswereanalyzedusingrepeatedmeasuresANOVAandcategoricaldatawerecomparedbytheχ2testorFisher'sexacttest.
SurvivalcurveswereestimatedbytheKaplan-Meiermethodwiththelog-ranktest.
Multivari-ateanalysiswasperformedusingtheCoxproportionalhazardregressionanalysis.
Pvalues<0.
05wereconsi-deredsignificant.
Table1Baselinecharacteristicsofthe80patientsControl(n=40)Ulinastatin(n=40)PAge56±1256±100.
861Gender(male/female)34/633/70.
762TNMstage(I/II/III)7/18/156/20/140.
897Lengthofresection(cm)10±4.
811±4.
00.
157Numberoflymphnodedissection11±4.
110±4.
60.
154Alcoholconsumption(yes/no)25/1523/170.
648Smoker(yes/no)21/1920/200.
823FEV1/FVC(%)85.
3±3.
385.
1±4.
30.
769ASAclassification(I/II)18/2217/230.
822Durationofoperation(min)206±44207±430.
918Durationofanesthesia(min)240±46242±440.
862Bloodlossduringoperation(mL)520±43518±620.
903Figure1Effectofulinastatinonrespiratoryindex.
Respiratoryindex(RI)intheulinastatingroup(U)wassignificantlylowerthanthatinthecontrolgroup(C)1hourafterone-lungventilation(T2)andthetimeofsternalclosure(T3;P<0.
05).
TheRIwascalculatedasamarkeroflungdamageusingthefollowingformulas:RI=[FIO2*(760–47)-PaCO2/0.
8]/PaO2.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page2of6http://www.
wjso.
com/content/11/1/84ResultsBaselinecharacteristicsofenrolledpatientsDuringaperiodof12monthsbetweenJanuary2007andDecember2007,80patientsundergoingesophagecto-mywereenrolledinthisstudy.
BackgroundfactorsforesophagealcancerpatientsarelistedinTable1.
Therewerenosignificantdifferencesbetweenthegroupsinaverageage,gender,TNMstage,lengthofresection,numberoflymphnodedissection,alcoholconsumption,smoking,ASAclassification,durationofoperation,dur-ationofanesthesia,andbloodlossduringoperation.
Typeofanesthesiawasthesamebetweenthetwogroups.
Therewerealsonosignificantdifferencesinperi-operativemanagement,includingtheusageofsteroidandelastaseinhibitor,infusionandnutritionalsupport,andNSAIDsandotheranalgesics,betweenthetwogroups.
EffectofulinastatinonrespiratoryindexRIbeforeoperationdidnotdiffersignificantlybetweenthegroups(groupUvs.
C,0.
29±0.
07vs.
0.
31±0.
06),andthereweresignificanttime-dependentchangesinRIvalueinbothgroups(P<0.
05,Figure1).
GroupUsho-wedsignificantlylowerRIvaluesthanthatofgroupC,bothat1hourafterone-lungventilation(T2)(0.
40±0.
09Table2EffectofulinastatinonpostoperativeclinicalcourseControl(n=40)Ulinastatin(n=40)PCardiovascularcomplications111Pulmonarycomplications810.
034Anastomosisleakage111Anastomosisstenosis101Woundinfection111Total1240.
034Death101DurationofICUstay(hours)45±2433±160.
01Lengthofhospitalstay(days)11±410±20.
170Figure2EffectofulinastatinonlymphocytesubsetsandIL-6.
Ulinastatin(U)administrationsignificantlyincreasedtherateofCD3+(A)andCD4+(B)cells,andratioofCD4+/CD8+(D),butdecreasedtherateofCD8+(C)cellsandreleaseofIL-6(E)comparedtocontrolgroup(C)onpostoperativedays1(D1)and3(D2;P<0.
05).
D0=1hourbeforesurgery,D3=Postoperativeday7.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page3of6http://www.
wjso.
com/content/11/1/84vs.
0.
53±0.
11,P<0.
05)andthetimeofsternalclosure(T3)(0.
75±0.
16vs.
0.
90±0.
17,P<0.
05).
EffectofulinastatinonpostoperativeclinicalcourseThepostoperativeclinicalcourseofeachpatientwascare-fullymonitoreddaily,andcomplicationswerechecked(Table2).
Postoperativecomplicationswereobservedin12patients(30%)intheCgroupand4patients(10%)intheUgroup,respectively(P<0.
05).
AsignificantdecreaseinpulmonarycomplicationswasobservedintheUgroup(P<0.
05),andonepatientintheCgroupdiedofpul-monaryoedema.
Althoughlengthofhospitalstayshowednosignificantdifferencesbetweenthetwogroups,thedurationofICUstaywassignificantlyshorterintheUgroup(P<0.
05).
AscanbeseenfromFigure2,ulinastatinadministra-tionsignificantlyincreasedtherateofCD3+andCD4+cells,andratioofCD4+/CD8+,butdecreasedtherateofCD8+cellsandreleaseofIL-6comparedtotheCgrouponD1andD2(P<0.
05).
SideeffectsNopatientexperiencedsideeffectsrelatedtoulinastatinadministration;namely,shock,itching,rash,nausea,vo-miting,orneutropenia.
SurvivalanalysisOf80patientsinthedatabase,onepatientdiedintheCgroupduringtheperioperativeperiod,and3werelosttofollow-up.
Asaresult,76patientswereenrolledforsurvivalanalysis.
TherecurrencerateoftheUgroupwas57.
5%comparedto72.
5%intheCgroup.
Themostcommonrecurrencepatternwaslocoregionalrecurrence(60%intheUgroupand72%intheCgroup),whileotherpatientsdevelopedsystemicrecurrenceoracom-binationofboth.
Recurrence-freesurvivalofallpatientswas33.
8±1.
7months,anditwasstatisticallybetterfortheUgroup(39.
4±2.
2)comparedtotheCgroup(27.
8±2.
4)byKaplan-Meieranalysis(P<0.
05,Figure3).
Multivariateanalysisrevealedthatulinastatinadminis-trationsignificantlydecreasedtheincidenceofrecur-rence(Table3).
DiscussionMajorstressfulsurgeryincludingesophagectomyalwayscausedoverproductionofproinflammatorycytokines.
Theinitialproinflammatoryresponsemaybeuncon-trolledcausinganimbalancebetweeninflammatoryre-sponsesyndromeandcompensatoryanti-inflammatorycytokineresponsesyndrome,whichledtopostoperativecomplications[15].
Forthespecialsurgicalprocedures,theriskofpulmonarycomplicationsafteresophagec-tomyishigherthananyothercommonoperation[16].
Moreover,surgicalstresscancauseimmunosuppressionFigure3Kaplan-Meiersurvivalanalysis.
CumulativerecurrencefreesurvivaldifferencesbetweenpatientsintheCandUgroups.
PatientswithintheCgroupshowedworserecurrencefreesurvival.
Pvaluewasobtainedusingthelog-ranktestofthedifference.
Table3MultivariatecoxproportionalhazardsanalysisforrecurrencefreesurvivalVariablesRecurrencefreesurvivalPRR95%CIUlinastatinadministration0.
1490.
063-0.
351<0.
05TNM1.
8120.
652-5.
0380.
254Alcoholconsumption2.
0660.
909-4.
3440.
757Smoking1.
0880.
534-2.
2170.
817Gender0.
9160.
425-1.
9730.
822Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page4of6http://www.
wjso.
com/content/11/1/84inresponsetooverproductionofproinflammatorycytoki-nes.
Inesophagealcancer,aprognosticrelationbetweenthepresenceofcomplicationsandimmunosuppressionafteresophagectomyandsurvivalhaspreviouslybeenreported[17,18].
Thesedatasuggestthataneffectivecountermeasureagainstpostoperativecomplicationsandimmunosuppressionisdesirable.
Ulinastatinhasmanyphysiologicaleffectsinsurgicalstress,includingthedecreaseoftheinflammatoryre-action,inhibitionofimmunosuppression,andmodifica-tionofthewaterbalance[13,19,20].
Moreover,previousstudieshaveshownthatulinastatininhibitshumanovar-iancancerandtheeffectcouldberelatedtodown-regulationofproteinkinaseC[21].
Studieshavealsofoundthatulinastatinenhancestheinhibitoryeffectofdocetaxelinbreastcancerbyamechanismconsistentwiththedown-regulatedexpressionofIL-6,IL-8,andTNF-α[22].
Sinceulinastatinhadapreventiveeffectonpostoperativecomplicationsandimmunosuppression,andmightinhibitthegrowthofcancercells,wechoseitforthecertainpurpose.
CD3+,CD4+,CD8+T-lymphocytepercentageandCD4+/CD8+ratiowerecloselyrelatedtothecellularim-munefunctionandpostoperativeanti-tumorimmunity[23-25].
Moreover,lowerCD3+,lowerCD4+andlowerCD4+/CD8+ratiowerefactorsindependentlyassociatedwithworseprognosisofesophagealcancerpatientsindifferentreports[26,27].
Therefore,weinvestigatedef-fectofulinastatinadministrationoncontentoflympho-cytesubsets.
Inthepresentstudy,itwasfoundthatulinastatinad-ministrationhadaprotectiveeffectonpulmonaryfunc-tionbydecreasingtheincreasingtrendofRIduringoperation.
Asaresult,thepostoperativecomplicationswerelowerthanthatintheCgroup,especiallyforpul-monarycomplications.
LowoccurrenceofpostoperativecomplicationsshortensthedurationofICUstayandde-creasedcostofcare.
Further,weinvestigatedtheeffectofulinastatinonreleaseofIL-6andcontentoflym-phocytesubsets.
Thechangeofpost-operativeIL-6andlymphocytesubsetsreflectedbeneficialeffectsofuli-nastatinonanti-inflammatoryaction,postoperativeim-munosuppression,andpostoperativeanti-tumorresponse.
Finally,weobservedthattheUgrouphadalongerrecur-rencefreesurvival.
ConclusionsFromtheseresultsweconcludedthatulinastatinhadapreventiveeffectonpostoperativecomplicationsandimmunosuppressioninesophagectomypatients,thereby,prolongingrecurrencefreesurvival.
Thepossiblereasonmaybethattheenhancedanti-tumorresponseinhibitedtumormetastasis[28,29].
However,thedetailedmecha-nismofactionofulinastatinshouldbefurtherstudiedatthemolecularbiologicallevel.
Evaluationofalargenum-berofcasesisalsonecessarytoassesstheclinicaluseful-nessofulinastatin.
AbbreviationsIL-6:Interleukin-6;RI:Respiratoryindex.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Authors'contributionsLMandNWparticipatedinthedesignandconductionofexperiments,dataanalysis,andfinaldraftingandwritingofthemanuscript.
LM,NW,SZandWYallcontributedtotheseexperiments.
GJandMZwerecloselyinvolvedinresearchdesignanddraftingofthefinalmanuscript.
Allauthorsreadandapprovedthefinalmanuscript.
Authordetails1DepartmentofAnesthesiology,FirstAffiliatedHospital,MedicalSchool,Xi'anJiaotongUniversity,Xi'an710061,ShaanxiProvince,China.
2DepartmentofAnesthesiology,SecondAffiliatedHospital,MedicalSchool,Xi'anJiaotongUniversity,Xi'an710061,ShaanxiProvince,China.
3DepartmentofRadiotherapy,TangduHospital,FourthMilitaryMedicalUniversity,Xi'an710038,ShaanxiProvince,China.
4DepartmentofGastroenterology,TangduHospital,FourthMilitaryMedicalUniversity,Xi'an710038,ShaanxiProvince,China.
Received:28October2012Accepted:26March2013Published:10April2013References1.
WhooleyBP,LawS,MurthySC,AlexandrouA,WongJ:Analysisofreduceddeathandcomplicationratesafteresophagealresection.
AnnSurg2001,233:338–344.
2.
SatoN,KoedaK,IkedaK,KimuraY,AokiK,IwayaT,AkiyamaY,IshidaK,SaitoK,EndoS:Randomizedstudyofthebenefitsofpreoperativecorticosteroidadministrationonthepostoperativemorbidityandcytokineresponseinpatientsundergoingsurgeryforesophagealcancer.
AnnSurg2002,236:184–190.
3.
SudaK,KitagawaY,OzawaS,SaikawaY,UedaM,AbrahamE,KitajimaM,IshizakaA:Serumconcentrationsofhigh-mobilitygroupboxchromosomalprotein1beforeandafterexposuretothesurgicalstressofthoracicesophagectomy:apredictorofclinicalcourseaftersurgeryDisEsophagus2006,19:5–9.
4.
YamaguchiY,HiharaJ,HironakaK,OhshitaA,OkitaR,OkawakiM,MatsuuraK,NagamineI,IkedaT,OharaM,HamaiY:Postoperativeimmunosuppressioncascadeandimmunotherapyusinglymphokine-activatedkillercellsforpatientswithesophagealcancer:possibleapplicationforcompensatoryanti-inflammatoryresponsesyndrome.
OncolRep2006,15:895–901.
5.
KhansariDN,MurgoAJ,FaithRE:Effectsofstressontheimmunesystem.
ImmunolToday1990,11:170–175.
6.
OgawaK,HiraiM,KatsubeT,MurayamaM,HamaguchiK,ShimakawaT,NaritakeY,HosokawaT,KajiwaraT:Suppressionofcellularimmunitybysurgicalstress.
Surgery2000,127:329–336.
7.
ShakharG,Ben-EliyahuS:Potentialprophylacticmeasuresagainstpostoperativeimmunosuppression:couldtheyreducerecurrenceratesinoncologicalpatientsAnnSurgOncol2003,10:972–992.
8.
MasudaT,SatoK,NodaC,IkedaKM,MatsunagaA,OguraMN,ShimizuK,NagasawaH,MatsuyamaN,IzumiT:Protectiveeffectofurinarytrypsininhibitoronmyocardialmitochondriaduringhemorrhagicshockandreperfusion.
CritCareMed2003,31:1987–1992.
9.
InoueK,TakanoH,YanagisawaR,YoshikawaT:Protectiveeffectsofurinarytrypsininhibitoronsystemicinflammatoryresponseinducedbylipopolysaccharide.
JClinBiochemNutr2008,43:139–142.
10.
UemuraK,MurakamiY,HayashidaniY,SudoT,HashimotoY,OhgeH,SuedaT:Randomizedclinicaltrialtoassesstheefficacyofulinastatinforpostoperativepancreatitisfollowingpancreaticoduodenectomy.
JSurgOncol2008,98:309–313.
11.
OnoS,AosasaS,MochizukiH:Effectsofaproteaseinhibitoronreductionofsurgicalstressinesophagectomy.
AmJSurg1999,177:78–82.
Zhangetal.
WorldJournalofSurgicalOncology2013,11:84Page5of6http://www.
wjso.
com/content/11/1/8412.
BaoP,GaoW,LiS,ZhangL,QuS,WuC,QiH:Effectofpretreatmentwithhigh-doseulinastatininpreventingradiation-inducedpulmonaryinjuryinrats.
EurJPharmacol2009,603:114–119.
13.
SatoN,EndoS,KimuraY,IkedaK,AokiK,IwayaT,AkiyamaY,NodaY,SaitoK:Influenceofahumanproteaseinhibitoronsurgicalstressinducedimmunosuppression.
DigSurg2002,19:300–305.
14.
D'JournoXB,MicheletP,MarinV,DiesnisI,BlayacD,DoddoliC,BongrandP,ThomasPA:Anearlyinflammatoryresponsetooesophagectomypredictstheoccurrenceofpulmonarycomplications.
EurJCardiothoracSurg2010,37:1144–1151.
15.
LinE,LowrySF:Inflammatorycytokinesinmajorsurgery:afunctionalperspective.
IntensiveCareMed1999,25:255–257.
16.
FergusonMK,DurkinAE:Preoperativepredictionoftheriskofpulmonarycomplicationsafteresophagectomyforcancer.
JThoracCardiovascSurg2002,123:661–669.
17.
LagardeSM,deBoerJD,tenKateFJ,BuschOR,ObertopH,vanLanschotJJ:Postoperativecomplicationsafteresophagectomyforadenocarcinomaoftheesophagusarerelatedtotimingofdeathduetorecurrence.
AnnSurg2008,247:71–76.
18.
TakagiK,YamamoriH,MorishimaY,ToyodaY,NakajimaN,TashiroT:Preoperativeimmunosuppression:itsrelationshipwithhighmorbidityandmortalityinpatientsreceivingthoracicesophagectomy.
Nutrition2001,17:13–17.
19.
ParkJH,KwakSH,JeongCW,BaeHB,KimSJ:Effectofulinastatinoncytokinereactionduringgastrectomy.
KoreanJAnesthesiol2010,58:334–337.
20.
SatoA,KuwabaraY,ShinodaN,KimuraM,IshiguroH,FujiiY:Useoflowdosedopamine,gabexatemesilateandulinastatinreducesthewaterbalanceandpulmonarycomplicationinthoracicesophagectomypatients.
DisEsophagus2005,18:151–154.
21.
KobayashiH,SuzukiM,TanakaY,HirashimaY,TeraoT:SuppressionofurokinaseexpressionandinvasivenessbyurinarytrypsininhibitorismediatedthroughinhibitionofproteinkinaseC-andMEK/ERK/c-Jun-dependentsignalingpathways.
JBiolChem2001,276:2015–2022.
22.
ZhaoX,SunX,GaoF,LuoJ,SunZ:EffectsofulinastatinanddocetaxelonbreasttumorgrowthandexpressionofIL-6,IL-8,andTNF-α.
JExpClinCancerRes2011,30:22.
23.
UchidaK,KusudaT,KoyabuM,MiyoshiH,FukataN,SumimotoK,FukuiY,SakaguchiY,IkeuraT,ShimataniM:RegulatoryTcellsintype1autoimmunepancreatitis.
IntJRheumatol2012,2012:795026.
24.
YuWK,LiWQ,LiN,LiJS:Mononuclearhistocompatibilityleukocyteantigen-DRexpressionintheearlyphaseofacutepancreatitis.
Pancreatology2004,4:233–243.
25.
ChenL,LinsleyPS,HellstrmKE:CostimulationofTcellsfortumorimmunity.
ImmunolToday1993,14:483–486.
26.
NozoeT,MaeharaY,SugimachiK:PreoperativesortingofcirculatingTlymphocytesinpatientswithesophagealsquamouscellcarcinoma:itsprognosticsignificance.
WorldJGastroenterol2005,11:6689–6693.
27.
GuoSJ,LinDM,LiJ,LiuRZ,ZhouCX,WangDM,MaWB,ZhangYH,ZhangSR:Tumor-associatedmacrophagesandCD3-zetaexpressionoftumor-infiltratinglymphocytesinhumanesophagealsquamous-cellcarcinoma.
DisEsophagus2007,20:107–116.
28.
SheuBC,HsuSM,HoHN,LinRH,TorngPL,HuangSC:ReversedCD4/CD8ratiosoftumor-infiltratinglymphocytesarecorrelatedwiththeprogressionofhumancervicalcarcinoma.
Cancer1999,86:1537–1543.
29.
BalkwillF:Cancerandthechemokinenetwork.
NatRevCancer2004,4:540–550.
doi:10.
1186/1477-7819-11-84Citethisarticleas:Zhangetal.
:Preventiveeffectofulinastatinonpostoperativecomplications,immunosuppression,andrecurrenceinesophagectomypatients.
WorldJournalofSurgicalOncology201311:84.
SubmityournextmanuscripttoBioMedCentralandtakefulladvantageof:ConvenientonlinesubmissionThoroughpeerreviewNospaceconstraintsorcolorgurechargesImmediatepublicationonacceptanceInclusioninPubMed,CAS,ScopusandGoogleScholarResearchwhichisfreelyavailableforredistributionSubmityourmanuscriptatwww.
biomedcentral.
com/submitZhangetal.
WorldJournalofSurgicalOncology2013,11:84Page6of6http://www.
wjso.
com/content/11/1/84
- D0www.236jj.com相关文档
- TS12A4514www.236jj.com
- Windowswww.236jj.com
- mTORC2www.236jj.com
- milswww.236jj.com
- digitalwww.236jj.com
- mediumwww.236jj.com
ProfitServer$34.56/年,西班牙vps、荷兰vps、德国vps/不限制流量/支持自定义ISO
profitserver怎么样?profitserver是一家成立于2003的主机商家,是ITC控股的一个部门,主要经营的产品域名、SSL证书、虚拟主机、VPS和独立服务器,机房有俄罗斯、新加坡、荷兰、美国、保加利亚,VPS采用的是KVM虚拟架构,硬盘采用纯SSD,而且最大的优势是不限制流量,大公司运营,机器比较稳定,数据中心众多。此次ProfitServer正在对德国VPS(法兰克福)、西班牙v...
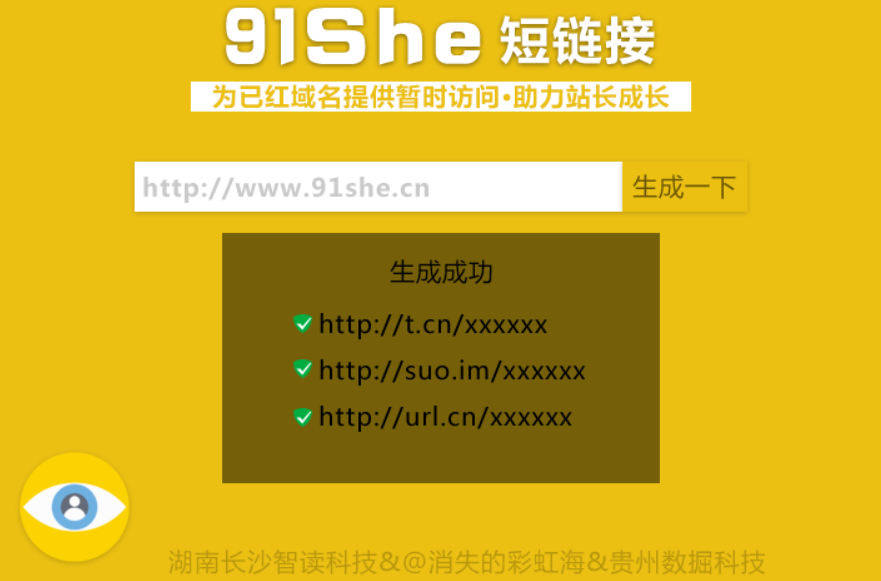
QQ防红跳转短网址生成网站源码(91she完整源码)
使用此源码可以生成QQ自动跳转到浏览器的短链接,无视QQ报毒,任意网址均可生成。新版特色:全新界面,网站背景图采用Bing随机壁纸支持生成多种短链接兼容电脑和手机页面生成网址记录功能,域名黑名单功能网站后台可管理数据安装说明:由于此版本增加了记录和黑名单功能,所以用到了数据库。安装方法为修改config.php里面的数据库信息,导入install.sql到数据库。...
酷锐云香港(19元/月) ,美国1核2G 19元/月,日本独立物理机,
酷锐云是一家2019年开业的国人主机商家,商家为企业运营,主要销售主VPS服务器,提供挂机宝和云服务器,机房有美国CERA、中国香港安畅和电信,CERA为CN2 GIA线路,提供单机10G+天机盾防御,提供美国原生IP,支持媒体流解锁,商家的套餐价格非常美丽,CERA机房月付20元起,香港安畅机房10M带宽月付25元,有需要的朋友可以入手试试。酷锐云自开业以来一直有着良好的产品稳定性及服务态度,支...

www.236jj.com为你推荐
-
汇通物流百世汇通快递需要多少运费汇通物流请大家千万不要使用汇通快递!!网络访问域名访问提示是什么意思编程小学生惊库克少儿编程,编程小将的班值得报吗?固态硬盘是什么固态硬盘是什么意思百花百游百花净斑方效果怎么样?mole.61.com摩尔庄园RK的秘密是什么?www.5any.comwww.qbo5.com 这个网站要安装播放器m88.comwww.m88.com现在的官方网址是哪个啊 ?www.m88.com怎么样?www.idanmu.com万通奇迹,www.wcm77.HK 是传销么?