resultantesetnod32id
esetnod32id 时间:2021-05-25 阅读:()
REVIEWOpenAccessGenerationofpancreaticβcellsfortreatmentofdiabetes:advancesandchallengesHussainMd.
Shahjalal1,2,AhmedAbdalDayem1,KyungMinLim1,Tak-ilJeon1andSsang-GooCho1*AbstractHumanembryonicstemcells(hESC)andinducedpluripotentstemcells(hiPSC)areconsideredattractivesourcesofpancreaticβcellsandisletorganoids.
Recently,severalreportspresentedthathESC/iPSC-derivedcellsenrichedwithspecifictranscriptionfactorscanformglucose-responsiveinsulin-secretingcellsinvitroandtransplantationofthesecellsameliorateshyperglycemiaindiabeticmice.
However,theglucose-stimulatedinsulin-secretingcapacityofthesecellsislowerthanthatofendogenousislets,suggestingtheneedtoimproveinductionprocedures.
OneofthecriticalproblemsfacinginvivomaturationofhESC/iPSC-derivedcellsistheirlowsurvivalrateaftertransplantation,althoughthisrateincreaseswhentheimplantedpancreaticcellsareencapsulatedtoavoidtheimmuneresponse.
SeveralgroupshavealsoreportedonthegenerationofhESC/iPSC-derivedislet-likeorganoids,butdevelopmentoftechniquesforcompleteisletstructureswiththeeventualgenerationofvascularizedconstructsremainsamajorchallengetotheirapplicationinregenerativetherapies.
ManyissuesalsoneedtobeaddressedbeforethesuccessfulclinicalapplicationofhESC/iPSC-derivedcellsorisletorganoids.
Inthisreview,wesummarizeadvancesinthegenerationofhESC/iPSC-derivedpancreaticβcellsorisletorganoidsanddiscussthelimitationsandchallengesfortheirsuccessfultherapeuticapplicationindiabetes.
Keywords:Embryonicstemcells(ESC),Inducedpluripotentstemcells(iPSC),Differentiation,Pancreaticβcell,Isletorganoids,Transplantation,βCellmaturationBackgroundDiabetesmellitusisalife-threateningdisease,anditsprevalenceisincreasingworldwide.
Theavailabletreat-mentcanneithercurenorcompletelycontrolthecom-plicationsofthisdisorder,whichresultsinsubstantiallossesoflifeinalmostallcountriesintheworld.
Fur-thermore,currentlife-longtreatmentstrategiesimposelargesocialandeconomicburdensonafamily.
Forthelastfewdecades,humanbeingshavebeentryingtode-velopatreatmentstrategythatcaneffectivelycontrolthisdisorderandsavelives.
Despitetremendousefforts,however,humanshavebeenfarfromsuccessinfindinganeffectivetreatmentstrategyfordiabetes.
Type1diabetesresultsfromanabsolutedeficiencyofinsulinduetoTcell-mediatedautoimmunedestructionofpancreasβcells[1].
Thecurrenttreatmentfortype1diabetesissolelydependentontheadministrationofex-ogenousinsulin.
Althoughthisapproachmanagesthedisease,unwantedrisksandlong-termcomplicationspersistbecauseoftheinabilitytotightlymaintainglucoselevelswithinanormalphysiologicalrange.
Complicationsincludelife-threateningepisodesofhypoglycemia,aswellaslong-termcomplicationsthatincludemicro-andmacro-angiopathyleadingtocardio-vascularpathologies,kidneyfailure,andneuropathy.
Thus,thereisaneedfornewtreatmentsthatprovidesuperiorcontrolofbloodglucosetominimizethesecomplications[2].
Oneexistingapproachtotreatingdia-betesistransplantationofpurifiedhumancadavericis-letsintotheportalveintoreplacethedestroyedβcellsofthepatients.
Thisproceduretypicallyresultsinbetterglycemiccontrol,canrenderpatientsinsulinindepend-entforprolongedperiodsoftime,andimprovesoverall*Correspondence:ssangoo@konkuk.
ac.
kr;ssangoo33@gmail.
comHussainMd.
ShahjalalandAhmedAbdalDayemcontributedequallytothiswork.
1DepartmentofStemCell&RegenerativeBiotechnologyandIDASI(IncurableDiseaseAnimalmodel&StemcellInstitute),KonkukUniversity,120Neungdong-ro,Gwangjin-gu,Seoul05029,SouthKoreaFulllistofauthorinformationisavailableattheendofthearticleTheAuthor(s).
2018OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355https://doi.
org/10.
1186/s13287-018-1099-3qualityoflife[3,4].
Althoughpromising,becauseofdif-ficultiessuchasthescarcityofcadavericdonorscom-paredtothelargenumberofdiabeticpatients,lowyieldoftransplantableisletsfromcadavericpancreases,andnecessityforchronicimmunosuppressiontopreventre-jectionoftheallograft[5,6],analternativesourceofsurrogatecellsisneeded.
Moreover,thenumberoffunc-tionalβcellsthatcanbeextractedfromasinglecadav-ericpancreasisoftennotenoughtorestoreeuglycemiainasinglediabeticpatient[7].
Thisalsoillustratestheneedforalternativesourcesofβcellstotreatthein-creasingnumberofdiabeticpatients.
Humanpluripotentstemcells(hPSCs),includinghu-manembryonicstemcells(hESC)andinducedpluripo-tentstemcells(hiPSC),areconsideredveryattractivealternativesourcesofsurrogateβcellsbecauseoftheirabilitytodifferentiateintoallmajorsomaticcelllineages[8,9].
Todate,themostsuccessinproducingpancreaticβ-likecellsfromhPSCshascomefromapproachesthatmimicnormalpancreasdevelopment.
Manyresearchgroupshavefollowedthisapproach,whichinvolvesex-posingthecellstovariousgrowthfactorsandsignalingmoleculesatspecificdosesandinaparticularsequencetosuccessfullydifferentiatethecellsintopancreaticendodermorendocrinecells(ECs)[2,10–29].
However,inmanystudies,alargenumberofpolyhormonalinsulin-expressingcellshavebeenobservedinculturethatresembletransientECsseeninmid-gestationhu-manfetalpancreases[10,11,15–17,30–32].
Thesepoly-hormonalcellslackexpressionofkeyβcelltranscriptionfactorsanddonotsecreteinsulininvitroinresponsetoglucosechallenge—thehallmarkfunctionofbonafideβcells[10,32–34](Fig.
1a).
Concurrently,inseveralotherstudies,analternativestrategyhasbeenadoptedinwhichglucose-responsiveinsulin-secretingcellscanbegeneratedfollowingtransplantationofhESC/iPSC-derivedpancreaticprogenitorcellsintoectopicsitesinimmuno-deficientortype1diabeticmice[12,14,18–21,26].
Inre-cipientmice,theresultingcellscanproducehumaninsulintoreversediabetes[18,20,21](Fig.
1b).
Inrecentyears,optimizeddifferentiationprotocolshavebeensuc-cessfullydevelopedtogenerateglucose-responsiveinsulin-secretingcellsinvitrofromhESC/iPSC,whichex-pressmatureβcellmarkers,andtransplantationoftheseabcFig.
1Differentiation,maturation,andfunctionofpancreaticβcellsderivedfromhESC/iPSC.
Insulin-positivepolyhormonalcellsmostlyformedinmanyinvitrocellcultureprotocolswhichshowlimitedornoGSIS(a).
Alternatively,EPcellswereformedfromhESC/iPSCinamonolayerand/orrotatingsuspensionculture,andtransplantationofthesecellsgeneratedislet-likeECsthatexhibitedGSISandcouldreversehyperglycemia(b).
Recently,pancreaticβ-likecellsexpressingmatureβcellmarkersandexhibitingGSISinvitroweregeneratedineitherlowadhesioncultureorrotatingsuspensionculture;aftertransplantation,thesecellsunderwentfurthermaturation,secretedinsulininresponsetoglucose,andamelioratedhyperglycemiaindiabeticmice(c).
GSIS,glucose-stimulatedinsulinsecretion;AFP,hepaticprogenitorcellsexpressingAFP;CDX2,intestinalprogenitorcellsexpressingCDX2;PP,pancreaticprogenitor;EP,endocrineprecursor;INS,β-likecellsexpressinginsulin;GCG,αcellsexpressingglucagon;SST,δcellsexpressingsomatostatinShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page2of19cellshasbeenshowntoamelioratehyperglycemiaindia-beticmice[2,22,23,29](Fig.
1c).
Theβ-likecellsgener-atedshowgeneexpression,ultrastructuralcharacteristics,andglucoseresponsivenessbothinvitroandinvivo,whichcloselyresemblingthefeaturesofβcellsfoundinpancreaticislets[2,22,23].
Inthesemultistageprotocols,thefinalcellpopulationhasabout30–60%β-likecells,andthemajorityoftheremainingcellsarerelativelyuncharacterizedcellsthatcanbeundifferentiatedprogeni-torsorothertypesofunwantedcells.
Thus,improvingef-ficiency,intermsofthepercentageofdifferentiatedcellsthatbecomeβcells,remainsanimportantchallenge.
Althoughtremendoussuccesshasbeenachievedinthelastfewyears,lowsurvivalratesofhESC/iPSC-der-ivedpancreaticcellsaftertransplantationintoectopicsitesinrecipientsremainacriticalproblem[20,25,35].
Therefore,anefficientculturesystemthatcanbeusedtogeneratefunctionalandterminallydifferentiatedβcells,alongwithaneffectivetransplantationtechnique,isneededforclinicalapplicationofhESC/iPSC-derivedβcellsfordiabetestreatment.
However,phase1/2clin-icaltrialsfortheapplicationofhESC-derivedpancreaticprogenitorsintype1diabetespatientshavealreadybegun[36].
Inthisreview,wesummarizeadvancesinthedifferentiationofhESC/iPSC-derivedcellsintopan-creaticβcellsandislet-likeorganoidsanddiscussthelimitationsandchallengesfortheirsuccessfulgenerationandtherapeuticapplicationintype1diabetes.
PluripotentstemcellsandtheirreprogrammingESCsshowunlimitedreplicativepropertiesandthepo-tentialtodifferentiateintoanyadultcelltype[37–39].
iPSCs,establishedfromsomaticcellsofmouseandhu-man[40–42],havethesameabilitytoexpandanddiffer-entiateasESCs.
Therefore,bothESCsandiPSCshavegreatpotentialforuseincelltherapies.
However,theuseofiPSCshasfewerethicalcomplicationsthanESCsthatarederivedfromtheinnercellmassoflivingembryos.
iPSCsarederivedfromvarioussomaticcellsafterexpos-uretoacombinationoftranscriptionfactorssuchasOct3/4,Sox2,Klf4,andc-Myc[40,41].
iPSCgenerationiscarriedoutviaviral-basedandnon-viral-basedmethodsassummarizedinFig.
2.
Thesemethodsarevariedintheirefficiencies,transductionperiod,genomeFig.
2GenerationofiPSCsfromvarioussomaticcells.
iPSCgenerationcarriedoutviaviral-basedandnon-viral-basedmethodsaresummarizedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page3of19integration,andcost[43–48].
Therefore,selectionofthereprogrammingmethoddeterminesthefurtherapplica-tionoftheproducediPSCinregenerativemedicine.
Generally,viral-basedmethodsleadtogenomeintegra-tionandareoflowsafety,albeit,thehighefficiency.
MostiPSCsaremadeusingretrovirusvectors,whichin-tegratereprogrammingfactorsintohostgenomes.
Retrovirusvectorscanspontaneouslyinfectvariouscelltypesandinserttheircodinggenesintohostgenomesusingreversetranscriptase,whichallowscontinuoustransgeneexpressionduringreprogramming.
RetroviraltransgeneexpressioncontinuesuntilthecellsbecomeiPSCs,andthen,theretroviralpromoterisinactivated,possiblybecauseofepigeneticmodificationssuchashis-tonemethylation[49].
Thisguidedreprogrammingandautomaticsilencingmechanismisconsideredveryim-portantforiPSCinductionfromsomaticcells.
Recently,severalvirus-freetechniqueshavebeendevelopedfortheproductionoffootprint-freeiPSCs;theirefficientculturetechniqueshavealsobeenestablished[50–57].
ESCsvs.
iPSCs:similaritiesanddifferencesSimilartoESCs,iPSCshaveacharacteristicmorphology,abilitytogenerateembryoidbodiesandteratomas,andunlimitedproliferationcapabilityinvitro,whiletheymaintaintheirpluripotencybyexpressingpluripotencygenes.
However,severalstudieshaverevealedsomedif-ferencesbetweenhESCsandhiPSCsintermsofgeneex-pressionprofiles[58],epigeneticmodificationssuchasDNAmethylation[59],geneticstability[60],imprintedgeneexpressionstability[61],differentiationpotentials[62,63],anddiseasemodeling[64].
iPSCshavesome"memory"oftheirsomaticoriginandthereforearenotidenticaltoESCs.
ThememoryofiPSCmayaffecttheirsafety[65].
However,thereisnosufficientevidenceyettodeterminewhetheriPSCmemorycanbefatalincelltherapies.
DifferentiationofhESC/iPSCintopancreaticβcellsInsulin-producingcellswithpancreaticβcellcharacter-isticswerefirstsuccessfullyderivedinembryoidbodiesfromspontaneousdifferentiationofhESC[66].
Sincethen,numerousmethodstogeneratepancreaticendo-dermorβ-likecellsfromhESC/iPSChavebeenreported[2,10–29].
Thesestudiesdemonstratedthegenerationofinsulin-positivecells,aswellasglucagon-andsomatostatin-positivecells(Table1).
However,theper-centagesofinsulin-positivecellsobtainedinculturevaryamongtheprotocols.
Thekeystagesofembryonicpancreasdevelopmentin-cludedevelopmentofthedefinitiveendoderm(DE),primitiveguttube(PG),pancreaticprogenitor(PP),endo-crineprogenitor(EP),andhormone-expressingECs.
Basedoninformationaboutembryonicpancreasdevelop-ment,eachdifferentiationprotocolhasbeendesignedtousevariouscytokinesorsignalingmodulatorsatspecificdosesandinparticularsequencestoactivateorinhibitkeysignalingpathways,includingnodal/activin,Wnt,PI3K,fibroblastgrowthfactors(FGF),bonemorphogeneticpro-tein(BMP),retinoicacid,hedgehog,proteinkinaseC,notch,epidermalgrowthfactor,andtransforminggrowthfactor-β(TGF-β).
Othergrowthfactorssuchasinsulin-likegrowthfactors1and2,hepatocytegrowthfac-tor(HGF),andglucagon-likepeptide-1(GLP-1)orexendin-4(apeptideanalogofGLP-1)havealsobeenusedtofacilitatedifferentiationofpancreatichormone-ex-pressingcells[10,11,13,15,16,24].
Inaddition,variousclassesofsmallmoleculeshavebeenreportedtobeeffect-ivefordifferentiationofhESC/iPSCintoinsulin-produ-cingcells.
Nicotinamide,apoly(ADP-ribose)synthetaseinhibitor,isusedinsomeprotocolstoimprovetheyieldofpancreaticECs[11,13,16,17,24].
Further,forskolin(anactivatorofadenylylcyclase)anddexamethasone(asyn-theticadrenocorticalsteroid)havebeenshowntoenhancecellularmaturation,andtheseagentscanbecombinedwithothersmallmoleculestoobtainsynergisticeffects[17].
Thyroidhormonepromotespostnatalβcelldevelop-mentandglucose-responsiveinsulinsecretioninratsthroughthetranscriptionfactorMAFA[67].
Thisinsighthasincreasedtheuseofthyroidhormoneinrecentproto-colstoimproveglucoseresponsivenessofhESC/iPSC-der-ivedβcells[22,23,25,27,28,68].
Severalreportshaverecognizedpancreaticprogenitorsco-expressingPancre-aticandDuodenalHomeobox1(PDX1)andNK6homeo-box1(NKX6.
1)asindispensableprecursorsofmaturepancreaticβcells[18,21,26].
Differentiationintopancre-aticprogenitorsco-expressingPDX1andNKX6.
1canbeenhancedinvitrobyeitherdissociatingdenselyformedendodermalcellsandre-platingthesecellsatalowdensityfollowedbyexposuretoalongerperiodofretinoidandFGF10signaling[68]orcultureswithhigh-densityag-gregates[26]orrotatingasuspensioncultureaftertheadditionoffactorssuchasALK5i(aTGF-βtypeIreceptorkinaseinhibitorII),TBP(aPKCactivator),and/orLDN(aBMPinhibitor)[18,21,23].
Theuseofepidermalgrowthfactor(EGF)andnicotinamideinthepancreaticprogenitorspecificationstagecanalsosignifi-cantlyenhancepancreaticprogenitorco-expressingPDX1andNKX6.
1[69].
MaturationofhESC/iPSC-derivedβcellsThematurationofpancreaticβ-likecellsobtainedbydifferentiationfromhESC/iPSCinvitroremainscontro-versial.
Intheearlystudies,eitherMatrigelorlow-densitymouseembryonicfibroblast(MEF)wasusedasa2DcultureplatformonwhichhESC/iPSCwereseeded[10,11,15–17,30–32].
TheseprotocolsShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page4of19Table1Generationofinsulin-positiveβ-likecellsfromhESC/iPSC,theirmaturation,andfunctionsinvitroandinvivoReferences[Celllinesused]DifferentiationconditionCelltypesinducedPercentinsulin+cellsGSISRecipients/transplantationsiteAmeliorationofhyperglycemiaD'Amouretal.
[10]CyT203[hESCline]Onlow-densityMEFsINS+,GCG+,SST+,PPY+,GHRL+7.
3%(3–12%)Non.
a.
n.
d.
Jiangetal.
[11]H1,H9[hESCline]OnMatrigelINS+,GCG+,SST+[n.
t:PPY+,GHRL+]>15%Yes(invitro)BALB/cnudemice/kidneycapsuleYesShimetal.
[12]Miz-hES4,Miz-hES6[hESCline]SuspensioncultureINS+,GCG+,SST+n.
d.
n.
d.
BALB/cnudemice/kidneycapsuleYesEshpeteretal.
[13]H1[hESCline]OnMatrigelINS+,GCG+,SST+5.
3%Yes(invivo)DiabeticC57BL6Rag1/1mice/kidneycapsuleNoKroonetal.
[14]CyT49,CyT203[hESCline]Onlow-densityMEFsINS+,GCG+,SST+,PPY+,GHRL+n.
d.
Yes(invivo)SCID-beigemice/epididymalfatpadYesChenetal.
[15]HUES-2,HUES-4,HUES-8,HUES-9[hESCline]Onlow-densityMEFsINS+,GCG+,SST+,[n.
t:PPY+,GHRL+]0.
8±0.
4%Low(invitro)CD1nudemice/kidneycapsulen.
d.
Zhangetal.
[16]H1,H9[hESCline];C1,C2,C5[hiPSCline]OnMatrigelINS+,SST+25%Yes(invitro)n.
a.
n.
d.
Kunisadaetal.
[17]253G1,201B7,297A1,297F1,and297L1[hiPSCline]Onlow-densityMEFsINS+,GCG+,SST+,GHRL+11.
8%(8.
0–16.
9%)Non.
a.
n.
d.
Rezaniaetal.
[18]H1,ESI-49[hESCline]Matrigel/suspensionculture(stirred)INS+,GCG+,SST+,PPY+~10%Yes(invivo)SCID-beigeandSTZ-diabeticmice/kidneycapsuleYesSchulzetal.
[19]CyT49[hESCline]Suspension(aggregates)INS+,GCG+,SST+,[n.
t:PPY+,GHRL+]n.
d.
Yes(invivo)SCID-beigemice/epididymalfatpadYesRezaniaetal.
[21]H1[hESCline]Matrigel/suspensionculture(stirred)INS+,GCG+,SST+,PPY+,GHRL+~55–60%(post-transplant)Yes(invivo)SCID-beigeandSTZ-diabeticmice/subcutaneouswithencapsulationdeviceYesBruinetal.
[20]H1[hESCline]Matrigel/suspensionculture(stirred)INS+,GCG+,SST+n.
d.
Yes(invivo)SCID-beigeandSTZ-diabeticmice/kidneycapsuleandsubcutaneouswithencapsulationdeviceYesShahjalaletal.
[24]Toe,201B7[hiPSC];KhES-3[hESCline]OnSynthemax(xeno-free)INS+,GCG+,SST+5–8%Yes(invitro)n.
a.
n.
d.
Rezaniaetal.
[22]H1[hESCline];anepisomalhiPSCPlanarculture/air-liquidinterfacecultureINS+,GCG+,SST+~50%Yes(invitroandinvivo)Non-diabeticandSTZ-diabeticmice/kidneycapsuleYesPagliucaetal.
[23]HUES8[hESC];hiPSC-1,hiPSC-2[hiPSCline]SuspensioncultureonastirplateINS+,GCG+,SST+>30%Yes(invitroandinvivo)SCID-beigeanddiabeticmice(NRG-Akita)/kidneycapsuleYesShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page5of19Table1Generationofinsulin-positiveβ-likecellsfromhESC/iPSC,theirmaturation,andfunctionsinvitroandinvivo(Continued)References[Celllinesused]DifferentiationconditionCelltypesinducedPercentinsulin+cellsGSISRecipients/transplantationsiteAmeliorationofhyperglycemiaRussetal.
[2]MEL1INSGFP/W[hESCline]Low-adherenceplatesINS+,GCG+,SST+~60%Yes(invitroandinvivo)STZ-diabeticNODmice/kidneycapsuleYesAgulnicetal.
[25]CyT49[hESCline]SuspensioncultureINS+,GCG+,SST+40–50%Yes(invivo)SCID-beigemice/subcutaneouswithencapsulationdevicen.
d.
Toyodaetal.
[26]KhES-3[hESCline];585A1,604B1,692D2,648B1and409B2[hiPSCline]OnMatrigel/lowadhesionplateINS+,GCG+,SST+n.
d.
Yes(invivo)NOD–SCIDmice/kidneysubcapsulen.
d.
Millmanetal.
[27]ND-1andND-2[NDhiPSCline];T1DhiPSClineOnMatrigel/SpinnerflasksonastirplateINS+,GCG+[n.
t.
.
:SST+]24–27%Yes(invitroandinvivo)ND-SCIDmiceandalloxan-induceddiabeticmice/kidneycapsuleYesManzaretal.
[28]T1DhiPSClineMatrigel/3DcultureINS+,GCG+,SST+~56%Low(invitro)ImmunodeficientSTZ-diabeticmice/shoulderregionYesYabeetal.
[29]TkDN4-M,253G1,454E2[hiPSCline]OnMatrigel/aggregateonultra-lowadhesionplateINS+,GCG+,SST+30–33.
6%Yes(invitro)STZ-diabeticNOD-SCIDmice/kidneycapsulesYesPercentagesofinsulin-positivecells,glucose-stimulatedinsulinsecretion(GSIS),andinvivofunctionsreportedfromvariousstudiesaresummarizedMEFs,mouseembryonicfibroblasts;INS+,insulin-positivecells;GCG+,glucagon-positivecells;SST+,somatostatin-positivecells;PPY+,pancreaticpolypeptide-positivecells;GHRL+,ghrelin-positivecells;n.
t.
,nottested;n.
a.
,notapplied;n.
d.
,notdeterminedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page6of19efficientlyestablishedPDX1+progenitorsbyusingretin-oicacidincombinationwithinhibitorsofBMPandhedgehogsignalingpathways,whilesimultaneouslyadd-ingeitherFGF10orFGF7.
Theβ-likecellsgeneratedinsuchmonolayerculturewerelargelypolyhormonalinsulin-expressingcells(Fig.
1a).
Polyhormonalcellslackexpressionofkeyβcelltranscriptionfactorsandexhibitlimitedglucose-stimulatedinsulinsecretion(GSIS)invitro[10,32–34].
Formationofnon-functionalpolyhor-monalcellsisconsideredthelimitationoftheseproto-cols.
Whetherthecultureplatformortheinappropriatecombinationsofgrowthfactorsintheculturemediapromotesuchcellsarenotclearlyknown.
Varyingde-greesofinvitroGSISfromhESC/iPSC-derivedinsulin-positivecellshavebeenreportedbyseveralstud-ies,includinganapproximately1.
7-foldincreaseob-servedbyChenetal.
[15],a2-foldincreasenotedbyJiangetal.
[11]andZhangetal.
[16],andapparentlynoGSISreportedbyD'Amouretal.
[10]andKunisadaetal.
[17](Fig.
1a)(Table1).
Thesedifferencesandlowlevelsofsecretedinsulincouldbeduetothegenerationofvaryingnumbersofpolyhormonalcellsinculture.
Thepolyhormonalcellsmayresembletheimmatureβcellsobservedinmid-gestationhumanfetalpancreases[70,71].
Theroleandfateofpolyhormonalcellsduringhu-manfetaldevelopmentarepoorlyunderstood;however,immunohistochemicalcharacterizationindicatesthatthesecellspossessanαcelltranscriptionfactorprofile[72].
Severalreportshavedescribedtheformationofglucagon-expressingαcellsinvivofollowingtransplant-ationofhESC-derivedpolyhormonalcells[21,33,73](Fig.
1a),anddynamicchromatinremodelingwasre-portedtooccurduringthistransitionintomaturedcelltypes[73,74].
StudiesofBruinetal.
[32]revealedsev-eralkeyfeaturesofpolyhormonalinsulin-positivecellsthatdifferfromthoseofmaturepancreaticβcells,in-cludingdefectsinglucosetransporterexpression,KATPchannelfunction,andprohormoneprocessingenzymes.
Thesedeficienciesmustbeaddressedwithfurtherproto-colmodificationstogeneratehESC/iPSC-derivedpan-creaticβcellsthatshowGSISinvitro.
AlthoughseveralofthesereportsdescribedthedetectionofGSISinvitro,noneofthereportedcellswerecapableofefficientlyre-storingeuglycemiainaninvivodiabeticanimalmodel.
Toovercomethislimitation,analternativestrategytoobtainglucose-responsiveinsulin-producingcellshasbeenestablishedinseveralstudies[12,14,18–21,26](Fig.
1b).
MostofthesestudiesusedMatrigelasthe2DplatformforESC/iPSCmonolayerculture,followedbysuspensionculturewithorw/ostirringusinglowadhe-sionplate.
Continuousstirringpromotescell-cellandcell-matrixinteractionswithintheculture.
TheresultantEPcellswerethentransplantedintorecipientmiceforfurtherdifferentiationinvivo.
ThesestudiesdemonstratedthathESC/iPSC-derivedpancreaticprogenitorcellswhentransplantedintoectopicsitesinimmunodeficientortype1diabetesmice;theyunderwentfurtherdifferentiationandmaturationintoglucose-responsiveinsulin-secretingcells,whichcouldreversediabetesinrecipientmice[18,20,21](Fig.
1b)(Table1),suggestingthatpancreaticpre-cursorsorimmatureislet-likecellsobtainedinvitrocouldmatureinvivo.
Thisalsoindicatesthatsomeinvivofac-torsarestillmissingininvitrogrowthfactorcocktails.
Therefore,growthfactorsandsignalingmoleculesin-volvedinpancreasdevelopmentneedtobebetterscreenedtodetecttheirpotentialabilitiestocausehESC/iPSCtodifferentiateintomaturepancreaticβcellsinvitro.
Inrecentyears,tremendoussuccesshasbeenachievedinestablishingdifferentiationprotocolsthatcangenerateglucose-responsiveinsulin-secretingβcellsfromhESC/iPSCinvitroexpressingmatureβcellmarkers,andameli-oratinghyperglycemiaindiabeticmicefollowingtrans-plantationofthesecells[2,22,23,29](Fig.
1c)(Table1).
Inthesestudies,hESCs/iPSCswereculturedeitherinlowad-hesionplateorinthree-dimensional(3D)suspensioncul-turewithcontrolledstirring,whichpromotecell-cellandcell-matrixinteractionsresultingintheformationofcellag-gregates.
Sequentialandtime-dependentuseofsignalingmoleculesinsuchculturesystemsconcurrentlyguideshESC/iPSC-derivedcellstoappropriatelydifferentiateto-wardspancreaticβcellswithbetterphenotypesinvitro.
Aftertransplantationintorecipientmice,cellsresidingintheaggregatesunderwentfurtherdifferentiationandmatur-ationintomatureβcells.
Thesesimplifieddifferentiationconditionsenabletheefficientgenerationofhumanpancre-aticandmorerestrictedendocrineprogenitorpopulationsfrompluripotentstemcellswithoutunwantedformationofpolyhormonalcells.
Furthermore,theinducedβcellsinthisprotocolshowbothinvitroandinvivogeneexpressionpatterns,ultrastructuralcharacteristics,andglucoserespon-sivenesstoinsulinsecretionthatcloselyresemblethoseofβcellsfrompancreaticislets[2,22,23].
Moreover,com-paredtopreviouslyreportedimplantationsofhESC/iPSC--derivedpancreaticprogenitors,forwhichittook3–4monthsafterimplantationforcellstomature,recentad-vancesinthegenerationofβcellsinvitrosubstantiallyshortenthewaitingtimetotherapeuticeffectsafterim-plantation.
Inastudy,Rezaniaetal.
[22]optimizedtheirpreviousdifferentiationprotocolbyaddingfactorssuchasvitaminC,proteinkinaseCactivators,transforminggrowthfactor-βreceptorinhibitors,andthyroidhormonestogen-erateinsulin-producingcellsataninductionrateofap-proximately50%.
Furthermore,theyidentifiedR428,aselectivesmall-moleculeinhibitoroftyrosinekinaserecep-torAXL,asacrucialfactorforthematurationofβcellsinvitro.
Pagliucaetal.
[23]alsooptimizedadifferentiationmethodtogenerateβcellsfromhESC/iPSCinvitroatanShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page7of19inductionefficiencyof>30%.
Inthisstudy,ascalablesuspension-basedculturesystemthatadoptedfromSchulzetal.
[19]wasusedtogeneratemorethan108hPSCsforfurtherdifferentiation.
Thisprotocoltakes4–5weeksandinvolvesauniquecombinationofsequentialculturestepsusingfactorsthataffectsignalinginnumerouspathways,includingsignalingbyWnt,activin,hedgehog,EGF,TGFβ,thyroidhormone,andretinoicacid,aswellasγ-secretaseinhibition.
Later,in2015,Russetal.
[2]showedthattheuseofBMPinhibitorstospecifypancreaticcellspromotestheprecociousinductionofendocrinedifferentiationinPDX1+pancreaticprogenitors,whichultimatelyresultsinthefor-mationofnon-functionalpolyhormonalcells.
Therefore,intheirculturesystem,thecommonlyusedBMPinhibitorswereomittedduringpancreaticspecification,whichpreventprecociousendocrineformation,whiletreatmentwithret-inoicacidfollowedbycombinedEGF/keratinocytegrowthfactor(KGF)efficientlygeneratesbothPDX1+andsubse-quentPDX1+/NKX6.
1+pancreaticprogenitorpopulations,respectively.
TheprecisetemporalactivationofendocrinedifferentiationinPDX1+/NKX6.
1+progenitorsfinallypro-ducesglucose-responsiveβ-likecellsinvitroataninduc-tionefficiencyof~60%.
Thus,thisprotocolisconsideredtobemorecloselyresembleskeyaspectsofearlyhumanpancreasdevelopmentand,assuch,representsanimprove-mentoverpreviousprotocols.
Alltheseobservationssug-gestthatinsulin-producingcellssuitablefordiabetescelltherapiescanbeproducedfromhESC/iPSCinvitro.
How-ever,theformationofhESC/iPSC-inducedβcellsinvitrodependsonmultiplefactors,suchastheuseofplatforms/materials,applicationofsuspensionculture,useofalargenumberofgrowthfactorsandtheircombinations,andthetimingofrotatingthecultures.
Inthesemultistageproto-cols,althoughthefinalcellpopulationhasonlyabout30–60%β-likecells,themajorityoftheremainingcellpopula-tioncomprisedrelativelyuncharacterizedcellsthatmaybeundifferentiatedprogenitorsorothertypesofunwantedcells.
Thus,improvingdifferentiationefficiencytogeneratehigherpercentagesofβcellsinvitroremainsanimportantchallenge.
AsimilariPSC-derivedβcellgenerationprotocolhasbeenreportedforpatientswithtype1diabetes(T1D)[27,28].
Millmanetal.
[27]reportedthattheinducedcellsexpressβcellmarkers,respondtoglucosebothinvitroandinvivo,preventalloxan-induceddiabetesinmice,andrespondtoseveralcategoriesofantidiabeticdrugs.
NomajordifferenceswereobservedinT1Dstemcell-derivedβcellscomparedtostemcell-inducedβcellsderivedfromnon-diabeticpatients.
Furthermore,T1DiPSC-derivedβcellsrespondedtodifferentformsofβcellstressinaninvitrodiseasemodel.
Manzaretal.
[28]generatedglucose-responsiveinsulin-producingcellsvia3Dculture.
Inthisstudy,T1DiPSCswereini-tiallyresistanttodifferentiation,buttransientdemethylationtreatmentsignificantlyenhancedtheyieldofinsulin-producingcells.
Thecellsrespondedtohigh-glucosestimulationbysecretinginsulininvitro.
Theshape,size,andnumberoftheirgranuleswereiden-ticaltothosefoundincadavericβcells.
Whentheseinsulin-producingcellsweretransplantedintoimmuno-deficientmicethathaddevelopedstreptozotocin(STZ)-induceddiabetes,hyperglycemiadecreaseddra-matically,sothatthemicebecomenormoglycemic.
Thus,T1DiPSC-derivedβcellsareasuitablecandidateforuseasanautologouscellsourceforthetreatmentofdiabetes.
However,amoreefficientculturesystemisre-quiredtogeneratefunctionalandterminallydifferenti-atedβcellsforfutureresearchandclinicalapplications.
IsletorganoidgenerationfordiabetestreatmentPancreaticisletsarecomposedofECs,includinginsulin-producingβcells,glucagon-producingαcells,somatostatin-producingδcells,pancreaticpeptide-pro-ducing(PP)cells,andghrelin-producingεcells[75–77].
Afterfunctionalmaturation,theseECsintheisletshelptoregulatebloodglucoselevels.
ReciprocalinteractionsamongECsintheisletsarecriticalforregulationofin-sulinsecretioninresponsetoglucose[78–80].
Thus,pancreaticisletstructuresofferaneffectivemeansofphysiologicallyregulatinginsulinsecretioninpatientswithdiabetesmellitus.
Organoidsareagroupofprimarycells,ESCs,oriPSCsgrowninvitrothatowetheirself-renewalcapacitiesandabilitytodifferentiateinto3Dstructuresthatassumeasimilarorganizationandfunctionalityasanorgan.
Thegenerationofisletorganoidscontainingmatureβcellswithfullfunctionalityisyettobedemonstrated.
How-ever,generatingsuchfunctionalorganoidswouldbevaluableinperformingpathologystudiesofdiabetesde-velopment,treatment,anddrugscreening[81,82].
Inthelastdecade,severalresearchgroupshavereportedonthegenerationofhESC/iPSC-derivedislet-likeclus-ters/aggregates,aswellasislet-likeorganoids[81–87].
Intheearlystudies,onlythefeasibilityofgeneratingislet-likeclustersoraggregatesfromhESC/iPSCwasstudied.
However,inrecentyears,considerablesuccesshasbeenachievedingeneratingislet-likeorganoids(Fig.
3).
Islet-likeorganoidsdevelopedfromhPSCbyKimetal.
[86]showedglucoseresponsivenessinvitro,aswellasinvivo.
Inthatstudy,ECsexpressingpancre-aticendocrinehormoneswerefirstgeneratedfromhESCandiPSCusingastep-wiseprotocol,andECclusters(ECCs)werethenformedspontaneouslyin1dayfromthedissociatedECsinanoptimized3Dculture.
ThesizesofthehESC-derivedECCswereapproximately50–150μmindiameter,whichissimilartothesizesofhu-manpancreaticislets.
TheECCscomprisedseveralpan-creaticECtypes,exceptforαcells,andthusshowedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page8of19thathESC-derivedECCsare,tosomeextent,analogoustohumanpancreaticisletsintermsofsizeandcellcom-position.
Levelsofβcell-associatedgenetranscriptionandGSISwerefoundtobehigherinECCsthaninECs.
Inaddition,intracellularCa2+influxoscillatedinECCsduringglucosestimulation,andSTZ-treateddiabeticmicetransplantedwithECCsbecamenormoglycemicwithin3daysaftertransplantationandsurvivedforap-proximately2months.
Thisstudy,therefore,supportedtheideathatfunctionalislet-likeorganoidscanbegener-atedfromhPSCs,whichcouldserveasanalternativesourceoftherapeuticcellsforthetreatmentofdiabetes.
AnotherstudybyWangetal.
[81]demonstratedthede-velopmentofisletorganoidsfromhESCin3Dbiomim-eticscaffoldsusingseveralgrowthfactors,whichpromotepancreaticECdifferentiation.
Theorganoidsformedinthisstudyconsistedofpancreaticα,β,δ,andPPcells,and,importantly,mostinsulin-secretingcellsgenerateddidnotco-expressglucagon,somatostatin,orPP.
Matureβcellmarkergeneswereexpressed,andinsulin-secretorygranules,whichareindicationsofβcellmaturity,weredetectedinthese3D-inducedcellclus-ters.
The3D-inducedorganoidcellsweresensitivetoglucoselevels;exposingthecellstoahighconcentrationofglucoseinducedasharpincreaseininsulinsecretion.
However,theseisletorganoidswerenottransplantedintoanimalmodelstoconfirmtheirbiologicalfunction.
Theconventional2Dcultureofstemcellsoverseveralpassagesinfluencecellphenotypeandfunction[88].
Cellsareonlypartiallypolarizedonaflatsubstrate.
Incontrast,3Dcellcultureonaspecializedmatrixpreventscellsfromattachingtothebottomoftheplatebymain-tainingthecellsinsuspensionorembeddingtheminthematrixinwhichcell-cellandcell-matrixinteractionsaremaintained,therebypromisesphenotypicmainten-anceandself-assemblyoffunctionaltissue-likepolarizedstructures[89–91].
3Dplatformsrecapitulatemechan-icalandbiochemicalstimuliaspresentinnativetissueandthusdictatepolarization[92].
However,suchstruc-turesoftendonotentirelymatchmulticellularorganizationseeninnativetissue.
Extracellularmatrix(ECM)isacriticalregulatorofcellularprocesseswhichservediversefunctionssuchassequesteringsignalingmoleculesandtransmittingligand-specificcuesviacellreceptorsandisamenabletosynthesis,degradation,andreassemblyovertime[93].
Cellsreadilyshapeandre-modeltheirextracellularenvironmentbyenzymaticallydegradingandresynthesizingtheECM.
Intissues,ECMnotonlyactsasanimmobilizationplatformforahigherorderofself-assemblybutalsofacilitatestherelayofabFig.
3Schematicoffabricationprocessesforislet-likeorganoids,adoptedandmodifiedfromCandielloetal.
[82]andTakahashietal.
[87].
aGenerationofhESC-derivedisletspheroidsandislet-likeorganoidsonAmikagelhydrogelplatform.
Pre-differentiatedhESC-derivedpancreaticprogenitorcells(hESC-PPs)on2DMatrigelwereharvestedandthenseededontotheAmikagelhydrogelplatformtoeitherformhomogenousisletspheroidsorbecombinedwithendothelialcells(HUVEC)toformendothelializedheterogeneousislet-likeorganoids.
Severalotherscaffold-basedstrategieshavealsobeenappliedtogeneratehESC-derivedislet-likeorganoidssuchascollagen-Matrigelscaffolds.
bGenerationofvascularizedislet-likeorganoidsinself-condensationculture.
Inthisprocess,isolatedadultmouse/humanisletsorhiPSC-derivedpancreatictissueswereco-culturedwithendothelialcells(HUVECs)andhumanmesenchymalstemcells(hMSCs).
Inthebeginning,thecellswerescatteredthroughouttheculturewell,andthen,theybeganmovingtowardsthecenterofthewelltoformcondensedtissue.
EachcondensedtissuecontainedpancreaticisletswithendothelialcellssurroundingthemShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page9of19biochemicalandmechanicalcuesinabufferedandhy-dratedenvironment[93].
ECMinteractionshavebeenshowntoimproveβcellproliferation[94],insulinsecre-tion[95,96],andisletdevelopment[96–98].
Collagenhasbeenusedwidelyfor3Dstemcellcultures[99].
Acollagenscaffoldconstitutesasoftandflexiblefibrousnetworkthatmaintainscellmorphologyandallowscellstofreelyreachout,migrate,andform3Dstructures.
However,collagenaloneisinsufficienttoprovidemul-tiplecuesandsophisticatedgeometryandcompositionthatexistinanativeextracellularmatrix.
Inpreviousstudies,thecombinationofcollagenwithMatrigel,acomplexheterogeneousmixtureofbasementmembraneproteinssuchaslaminin,collagenIV,fibronectin,hep-arinsulfateproteoglycans,andentactin,hasbeenusedastheunderlyingmaterialtoreconstructcardiacmuscleanduterinetissuesinvitro[100,101].
Inastudy,Wangetal.
[81]usedafour-stagedifferentiationstrategytodifferentiatehESCintopancreaticendodermandtoma-turethesecellsintoisletorganoidswithincollagen-Matrigelscaffolds.
Theirresultsshowedthataugmenta-tionofcollagenscaffoldswithMatrigelcreatesbetter3DnichesforisletorganoiddevelopmentfromhESC.
Al-thoughneitherMatrigelnorrattailcollagenIisaUSFoodandDrugAdministration-approvedmaterialforclinicalapplications,thestudyonlydemonstratedthefeasibilityofgeneratingisletorganoidsfromhESC.
How-ever,thecellclusterscanbepurifiedbyenzymaticallydigestingthescaffolds.
AnotheralternativeistouseaporcinedecellularizedECMtoconstructscaffolds.
Ashortageofdonorisletsiscurrentlylimitingthewide-spreadimplementationofislettransplantationtotreatdia-betes[102].
Inresponsetotheseneeds,recentstudieshavefocusedprimarilyonderivingisletβcellsfromhESC/iPSCasanalternativetodonorislets[2,22,23,27–29].
Thenon-endocrinecomponentsofisletsalsoplayacriticalroleintheirfunction.
Previously,heterogeneouspancreaticorganoidshavebeengeneratedbyaggregatingadultmouseβcellswithendothelialandmesenchymalcells[103].
Theseorganoidswerefoundtosuccessfullyintegratewithhostvasculatureandnormalizebloodglucoseindiabeticmice.
Systematicgenerationofheterogeneousorganoidsinvitrorequiresanorgan-specificcellsourceanda3Dcultureplat-formtoinduceself-organization,lineagespecification,func-tionalmaturationoforgan-specificcells,andintegrationofsupportingcellpopulations[104,105].
Scaffold-basedstrat-egieshaveprimarilyreliedonlaminin-richMatrigel,aswellasothernaturalorsyntheticbiomaterials,whichtypicallyconfinedcellswithinthe3Dscaffold.
Recently,isletorga-noidshavebeengeneratedfromhPSCsbyaggregatingthesecellsintohomogenous3Dislet-likespheroidsusing2Dnon-adherentculture[86]orbyembeddingtheminacollagen-Matrigelmatrix[81].
Effectivebioengineeredplat-formsthatwillsupportspecificorganoidproduction,finecontrolovertheorganoidsizeandcellularcomposition,scalingupofproduction,andeaseoforganoidrecoveryafterculturearestillneeded.
Hydrogelshavebeenafavoredchoiceofmaterialsintissueengineeringapplicationsduetotheirabilitytomimicthearchitectureandmechanicsofpli-ablecellularmicroenvironment[106,107].
Tissue-likeflu-idity,faciletransportofsolublenutrients,easeoffabrication,andintegrationwithbiologicalinterfacesaresomeofthemainadvantagesofahydrogelsystem.
Inare-centstudy,isletorganoidsofaprecisesizeandcellularhet-erogeneitywereengineeredfromhESC-derivedpancreaticisletcellsutilizinganovelhydrogelplatform,Amikagel[82](Fig.
3).
TheAmikagel-basedplatformwasshowntofacili-tatecontrolledandspontaneous,ratherthanforced,aggre-gationofhESC-derivedpancreaticprogenitorcells(hESC-PPs)intorobusthomogeneousspheroids.
Thefor-mationofAmikagel-inducedhESC-PPspheroidsenhancedpancreaticislet-specificPDX1andNKX6.
1geneandpro-teinexpression,whilealsoincreasingthepercentageofcellsco-expressingboth.
Amikagelalsoenabledco-aggregationofhESC-PPwithsupportingendothelialcells,resultinginself-organizedmulticellularpancreaticorganoidsthatwereclosertoisletphysiologyintermsoftheirheterogeneitythanhPSC-PPhomogenousspheroids.
.
TheseAmikagel-in-ducedhESC-PPspheroidsandheterogeneousorganoidsspontaneouslydifferentiatedintomatureβ-likecellsthatshowexpressionoftheβcell-specificINS1gene,aswellasC-peptideprotein,andproduceinsulininresponsetoinvitroglucosechallenge.
Aftermaturation,theAmikagel-in-ducedheterogeneousorganoidsalsoshowasignificantlydevelopedextracellularmatrixsupportsystem.
Therefore,theAmikagelplatformcouldbeidealforengineeringmulti-cellular3DisletorganoidsfromhPSCs.
Thepurposeforin-ducingandmaintaining3D-aggregatedorganoidsistoenhancetissue-ororgan-specificfunctionsbyreproducingcells'nativeenvironments.
Commonlyusedtechniquesforengineeringisletspheroidsneitherhaveprecisecontrolovertheultimatesizeofanaggregate,nordotheysupportcellinclusion,whichisthenextstepneededtogenerateisletorganoidswithmulticellularcomplexityandeventualgenerationofvascularizedconstructs.
TheAmikagelplat-formisparticularlysuitableinthiscontext.
Adevelopedextracellularmatrixbaseisimportantforisletstructure,cellhealth,andoverallfunction,whilealsobeingaprerequisiteforadevelopedvascularsystem[108].
Integrationofendothelialcellswouldbeanim-portantinitialsteptowardsvasculardevelopment[109].
Inthecontextofregenerativemedicine,tissuesurvivalandneovesselorganizationofhESC-derivedcellsmaybedependentonendothelialinclusionandmesenchymalsupplementation[110].
In2018,acomplexorganoiden-gineeringmethodtogeneratepancreaticisletswasre-ported[87](Fig.
3).
Usingthisprotocol,pancreaticislet-likeorganoidswithvascularnetworkswereformedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page10of19byco-culturingeitherisolatedadultmouse/humanislettissuesorhiPSC-derivedpancreatictissueswithvascularendothelialcells(HUVECs)andhumanmesenchymalstemcells(hMSCs).
Pancreaticislet-likeorganoidsweregeneratedbyself-condensationafterseedingcellsontotheMatrigelbed.
Transplantationofthesevascularizedislet-likeorganoidsintothekidneysubcapsuleoffulmin-anttype1diabeticmicesignificantlyimprovedthesur-vivalofthediabeticmiceandeffectivelynormalizedbloodglucosecomparedtoconventionalislettransplant-ation.
Thisapproach,therefore,offersapromisingalter-nativetotherapeuticislettransplantation.
Thefunctionalityofisletorganoidsgeneratedsofarremainspartial.
Someofthelimitationsoftheseorganoidsarethattheyoftenlackcelltypesneededforcompleteisletfunctionsandthegenerationofbloodvesselsandnerves.
Toapplyisletorganoidstothetreatmentofdia-betes,morecompleteisletstructuresmustbepreparedforbetterfunctionindiabeticrecipients.
Despitethepromiseofemergingisletorganoid-basedapproaches,developingvascularnetworksremainsamajorchallengetotheirapplicationinregenerativetherapies.
ESC/iPSC-derivedβcellsfordiabetestreatment:limitationsandchallengesTherearestillmanypointstoaddressandproblemstoovercomebeforehESC/iPSC-derivedcellscanbeclinic-allyappliedindiabeticpatients,includingthefollowing:(1)Safetyissues:Sofar,mostpatient-specificiPSCshavebeenestablishedwithretrovirusvectors.
TheseiPSCshavenumeroustransgeneintegrationsintheirgenomes,andtheseintegrationsmaycauseleakyexpressionthatcaninterruptthefunctionofendogenoustranscriptionfactornetworksandleadtodifferentiationfailure.
An-otherimportantproblemoftransgeneintegrationistumorigenicriskaftertransplantation.
Inparticular,c-Myc,oneofthereprogrammingfactors,isawell-knownoncogene,anditsreactivationcangiverisetotransgene-derivedtumorsinchimericmice[111].
TomakesafeiPSCs,oneimportantapproachmaybeelim-inatingthec-Myctransgeneinthereprogrammingcock-tail.
HumanandmouseiPSCscanbeestablishedfromfibroblastswithonlyOct3/4,Sox2,andKlf4,butboththeefficiencyofiPSCgenerationandthequalityofthesecellsaresignificantlyreduced[112].
Chimericmicepro-ducedwithc-Myc-freeiPSCsdidnotshowenhancedtumorformationincomparisonwithcontrolmice.
How-ever,retroviralinsertionsinthegenomeitselfmaydis-turbendogenousgenestructureandincreasetheriskoftumors[113].
ToincreasethesafetyofhiPSC-basedcelltherapies,itisnecessarytogeneratehiPSCswithoutvec-torintegrationandcontinuousc-MYCexpression.
ThegenerationofhiPSCswithtransientexpressionfromnon-integratingvectors[52,56,114]mayaddresstheseconcerns.
Todate,variousintegration-freetechniqueshavebeenreported,includingtransientexpressionofre-programmingfactorsusingadenovirus[115]orSendaivirusvectors[116],thepiggyBacsystem[51],episomalvectors[52,56],aminicirclevector[53],anddirectde-liveryofprotein[50]orsyntheticRNA[54].
However,theiriPSCinductionefficienciesarelowerthanthosewithretrovirusvectors,possiblybecauseoflowtrans-ductionefficiencyandunstableexpression[117].
(2)Variationindifferentiationefficiencies:DifferentiationpropensitiesarereportedtovaryamonghESClines[118].
Dependingonthecelloriginorderivationproced-ure,someiPSClinesalsodemonstratevaryingdegreesofdifferentiationefficiency,resistancetodifferentiation,ortumorigenicity[65,84].
Abnormalitiesinkaryotypeandvariationsinthetechniquesusedtoobtainormain-tainiPSClinesandepigeneticdifferencesamongthemhavealsobeenconsideredvitalfactorsthatalterdiffer-entiationpotential.
Epigeneticvariationsaremorepro-nouncediniPSCthanESC.
Thus,selectionofgoodiPSClineswithlowbatch-to-batchvariationindifferen-tiationefficiencyisessentialtodifferentiatingthesecellsintotargetlineagespriortouseinspecificcelltherapies[118].
Inaddition,differentiatedcellspreparedfrompatient-specificiPSCcanincreasethesuccessrateofcelltherapiesinthefuture.
(3)Formationofpolyhormonalcells:Polyhormonalinsulin-expressingcellsarefre-quentlyformedfromhESC/iPSC-derivedcellsinvitro,asdiscussedabove.
AvailablereportssuggestthatoncehESC/iPSC-derivedcellsbecomepolyhormonal,theycannotbedifferentiatedintomatureβcells[33].
There-fore,itisnecessarytofindouttherightcombinationoffactorstoreducetheformationofpolyhormonalcellsinculture,aswellastoinducethesecellsintomatureβcellsiftheyaregenerated.
(4)Xenogeneiccontamina-tionsandunknowneffects:Althoughmostrecentdiffer-entiationprotocolshavebeendevelopedonfeeder-freeculturesystems,manyprotocolsstillcallforavarietyofundefinedanimal-derivedproductsthatmayhaveun-knowneffectsoncellcharacteristicsanddifferentiationability.
Thepotentialconsequencesoftransplantinghu-mancellsexposedtoanimal-derivedproductsintopa-tientscouldincludeincreasedriskofgraftrejection,immunoreactions,microbialinfectious,prions,andyetunidentifiedzoonoses[119–121].
Toreducetheeffectsofxenogeneiccontamination,Micallefetal.
[122]usedxeno-freemedia;however,theyusedMEFforpassaging.
Inanotherstudy,Schulzetal.
[19]expandedhESCinxeno-freemediawithoutfeedercells,buttheyusedfetalbovineserumduringdifferentiation.
Later,Shahjalaletal.
[24]expandedanddifferentiatedhESCandiPSCinasyntheticscaffoldundercompletelyxeno-freeconditionsusingrecombinantand/orhumanizedcomponentsandsuccessfullygeneratedinsulin-expressingcellsinvitro.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page11of19ThesestudiesindicatethefeasibilityofgeneratinghESC/iPSC-derivedpancreaticβcellsunderxeno-freecondi-tions.
Forsuccessfulclinicalapplications,hESC/iPSCshouldbeprepared,maintained,anddifferentiatedinxeno-freeculturesystems.
Humanizedand/orrecombin-antfactors,chemicallydefinedsupplements,andsyn-theticscaffoldscanbeappliedinvitrotoaddressthisissue.
(5)Lackofmaturation:Todate,insulin-expressingcellsgeneratedfromhESC/iPSCinvitrolacktheproper-tiesofmaturepancreaticβcells.
Transplantationofim-maturehumanislet-likecellstoimmunodeficientmiceenablesfurthermaturationofisletcells.
Thisisevi-dencedbyhumanC-peptidesecretioninglucosetoler-ancetestsandbymorphologicalandultrastructuralstudies[2,22,23,123].
Itisimportanttounderstandwhatfactorsintheinvivomilieuarecriticaltofunc-tionalmaturation.
Thesecouldberelatedtolocalsignalsprovidedbytheinvivonicheatthetransplantsite.
Re-cently,ithasbeenshownthatmaturationoccursfasterandmoreefficientlyinfemalerecipientmice,pointingtothepotentialroleofestrogenreceptorsignalinginmaturation[124].
Geneprofilingstudiessuggestthatthecreationofmatureβcells,inwhichinsulinsecretionistightlycoupledtoglucoseconcentrations,requiresthecoordinatedupregulationofcertaingenesandrepressionofothers[125].
Arecentreportshowedthatligand-dependenttranscriptionfactorestrogen-relatedreceptor-γ(ERRγ)isadriveroftheoxidativemetabolicgenenetworkinmatureβcellsandthatitspostnatalin-ductionorchestratesthemetabolicmaturationofβcells[123].
Thisreportalsoindicatedthatβcell-specificERRγ-deficientmiceareglucoseintolerantandfailtoappropriatelysecreteinsulininresponsetoglucosechal-lenge.
ERRγexpressionduringpostnatalβcellmatur-ationdrivesatranscriptionalprogramthatpromotesthemitochondrialoxidativemetabolismnecessaryforGSIS.
Assuch,promotingERRγexpressionandactivityduringthelatestageofhiPSCdifferentiationinvitroresultsinglucose-responsiveβcellsthatarecapableofrestoringbloodglucoseintype1diabeticmice.
Thus,futurestud-iestoimprovefunctionalmaturationofinsulin-expressingcellsshouldfocusonsignalingpath-waysthatregulatethematurationofpancreaticβcells.
(6)Lowsurvivalrateandimmunogenicity:Becauseofthelackofasuitabletransplantationtechnique,there-coveryofwell-demarcatedgraftsaftertransplantationintoectopicsitesinexperimentalanimalsandexamin-ationofglucoseresponsivenessofhESC/iPSC-derivedpancreaticcellsinvivoarestilldifficult.
Thiscouldbeduetoimmunerejectioninthehostanimals.
Atpresent,twodifferenttransplantationstrategiesareapplied:oneisdirectimplantationofhESC/iPSC-derivedpancreaticcellsintoectopicsites,andotheroneisimplantationofadevicecontaininginducedpancreaticcells(Fig.
4).
Inthefirstmethod,pretreatmenttoinduceangiogenesisatimplantationsitesisusedtopromoteengraftmentandlong-termsurvivaloftheimplantedcells.
Onerecentstudyshowedthatanyloncatheterembeddedintothesubcutaneoustissuesofhostmicefor1monthbeforecellimplantationgeneratedavascularizedspace[126].
Theformationofvascularnetworksattheimplantationsiteandtheimplantationofpancreaticcellsafterinflam-matoryreactionshavediminisheddevelopealessin-tolerantenvironmentfortheimplantedcells.
Inthesecondmethod,pancreaticcellsareencapsulatedinadevicemadeofbiocompatiblematerialthatincludessemipermeablemembranes.
Oxygenandnutrientscanpassthroughthemembranestopromotecellsurvival,differentiation,andmaturation,whereasimmunemole-culesandcellscannot.
Severalstudieshaveshownthat,whenimplantedsubcutaneouslyintohostmice,hESC/iPSC-derivedpancreaticcellsencapsulatedbythesesemipermeablemembranedevicescanfurtherdifferenti-ateintomatureinsulin-secretingcellsandsurvivefromhostimmuneresponses,primarilybyTcells[20,21,25,35].
Inaddition,becauseofvasculogenesisaroundthesedevices,thedifferentiatedβcellscansecreteinsulininresponsetochangesinglucoseconcentrations.
ArecentstudyalsodemonstratedimplantationofhESC-derivedβ-likecellsencapsulatedwithanalginatederivative.
Thisdevicemitigatesforeignbodyresponsesandimplantsfi-brosis,andinducesglycemiccorrectionwithoutim-munosuppressioninimmune-competentmice[127].
Thesedevice-basedimplantationmethodscanreduceoreliminatetheneedforimmunosuppressiveagents.
Fur-thermore,thesemethodsmayhavetheadvantageofallowingremovaloftheimplantedcellswiththedevicewhenadverseeventssuchastumorigenesisordysfunc-tionoccur.
However,itispresentlyunclearwhetherpro-tectionfromsolubleantibodiesdirectedagainstdifferentiatedβcellswillbeasignificantproblem[128].
Althoughinsulin-expressingcellmaturationcanoccurwithorwithouttheimplantedcell/devicecombination,thesurvivalrateoftheimplantedcellsinhostsisstillrelativelylow.
Thus,asuitabletransplantationtechnique,alongwithaneffectivecombinationofinducers,isre-quiredtoovercomethistransplantationchallenge.
Des-piteseverallimitations,phase1/2clinicaltrialshavealreadystartedforthetreatmentoftype1diabetespa-tientsusingasemipermeablemembranecapsuledevicethatcarrieshESC-derivedpancreaticprogenitorsco-expressingPDX1andNKX6.
1[36].
Thistrialhasattractedattentionworldwide,asitrepresentsanim-portantfirststepforthedevelopmentofnewstemcelltherapiesfordiabetes.
Todate,noclinicaltrialswithhiPSC-derivedpancreaticcellshavebeencarriedout.
However,thepotentialadvantagesofhiPSCoverhESCmaymakesuchtherapiesavailableinthefuture.
(7)IsletShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page12of19βcellheterogeneity:βcellsinhumanpancreaticisletshavebeenthoughttobeahomogenouscellpopulation.
Despitethisprevailingparadigm,therehavealsobeenreportsofβcellheterogeneityinhumanislets[129,130].
Recently,astudybyDorrelletal.
hasidentifiedfourantigenicallydistinctsubtypesofhumanβcells,whicharedistinguishedbydifferentialexpressionofST8SIA1andCD9[131].
Theseβcellsubpopulationsarealwayspresentinnormaladultisletsandhavedi-versegeneexpressionprofilesanddistinctbasalandglucose-stimulatedinsulinsecretion.
Dissimilarbasalandglucose-stimulatedinsulinsecretioncharacteristicsindicatethattheβcellsubtypesarefunctionallydistinct.
Dorrelletal.
intheirstudyisolatedlivepancreaticβcellsfromhumanisletsamplesbyFACSandco-labeledthemwithantibodiesrecognizingST8SIA1andCD9andfi-nallyidentifiedfourantigenicallydistinctβcellsubpopu-lations.
TheyalsoaccessedtheexpressionofST8SIA1andCD9insectionsofhumanpancreasandfurtherconfirmedtheexistenceoffourdistinctβcellsubpopulationsinhumanislets.
TranscriptomeanalysesbyRNAsequencingoftheβcellsubsetshaveshownthatmostofthedifferentiallyexpressedgenesareofun-knownfunctioninβcells,butsomehavebeenclearlyassociatedwithinsulinsecretionorareknowntobedys-regulatedintype2diabetesmellitus.
Dorrelletal.
havealsoobservedthatthefrequenciesofβcellsubtypesarealteredinthemajorityofindividualswithtype2dia-betes.
Thus,theβcellsubpopulationsmayhaverele-vancetodiabetesandthisissueneedstobeaddressedbyextensiveresearch.
AlmostallpreviousstudieshaveattemptedtogeneratematureβcellsfromhumanESCs/iPSCs.
Recently,researchersaremainlyfocusingoneffi-cienttechniquestoenhancetheyieldofmatureβcellsandtheirsuccessfulsurvivalpost-transplantationtore-tainnormoglycemiaindiabetes.
However,βcellhetero-geneityisanemergingissue.
Thedistinctpropertiesofhumanβcellsubtypesfoundinhumanisletslikelyhaveanimportantimpactonmetabolicregulationandhu-mandiseaseprocesses.
Thus,futurestudiesshouldfocusabFig.
4MethodsforimplantinghESC/iPSC-derivedpancreaticcells.
Twodifferentmethodshavebeenapplied.
Inonemethod,hESC/iPSC-derivedpancreaticcellsareimplanteddirectlyintotransplantationsitesorintopre-developedvascularizedsitesofdiabeticand/ornon-diabeticSCIDmice(a).
Inanothermethod,hESC/iPSC-derivedpancreaticcellsencapsulatedinimmunoprotectivesemipermeabledevicesareimplantedintoectopicsitesofSCID-Beigeand/ordiabeticmice(b).
Oxygen,nutrients,insulin,andglucosecanpassthroughthemembranesofthedevicestopromotethesurvival,differentiation,maturation,andglucose-responsiveinsulinsecretionoftheencapsulatedpancreaticcellsfollowingimplantationintothehostmice.
Inaddition,vasculogenesisoccursaroundthedevices,supportingsecretionofinsulinfromthedifferentiatedβcellsinresponsetochangesinglucoseconcentrations.
Incontrast,immunecellsormoleculessuchasantibodiesandcomplementscannotpassthroughthemembranes,preventingimmunerejectionorautoimmuneresponsesagainstthecellsShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page13of19Table2StandardcriteriafordesigningandperformingfuturepreclinicalstudiesinvitroandinvivoPreclinicaltoolProsCons(challenges)Possibleimprovements-NODmouseisidealforstudyingtype1diabetesandthecharacterizationoftheimmunopathologyofthedisease.
-BioBreedingratisasuitablemodelforunderstandingthegeneticsoftype1diabetes[132]andstudyingofneuropathy-associateddiabetes[133].
-Diabetesinductioninthemurinemodelispossibleviatheexposuretocertainchemicals,namelystreptozotocinandalloxan,andthusoffersausefultoolfortestingthepotentialsoftherapeuticagentsortransplantedcellstoreduceglucoselevel.
-SomediseasesusceptibilitylociinNODmousehavenomarkedimpactinhumandisease.
-VariousdrugsandantibodytherapyshowedanexcellenteffectinNODmicebutnoeffectintheclinicaltrials[134].
-InductionofdiabetesinNODmiceiscorrelatedwithmicrobialinfections.
-Inductionofdiabetesusingchemicalsintheanimalmodelcouldshowtoxiceffectstotheotherorgans,suchasthekidney,liver,brain,intestine,andreproductiveorgans.
-Applyinghumanizedmousemodelhavingthecomponentsofthehumanimmunesystem.
-Takingintoaccountthegender-dependentdiabetespathogenicityinanimalmodels.
-Settingupnewanimalmodelsthatrecapitulatediabetespathogenesisinhuman.
-MaintainingNODmiceunderspecificpathogen-freeenvironmentduringdiabetesexperimentation.
-Consideringtoxicactionsinanimalmodelsduringthechemicalinductionofdiabetesinvivo.
PreviousreportsshowedtheoccurrenceoflymphopeniaandhighproductionofTregulatorycells[135].
-Forstudyingtype2diabetes,theoccurrenceandthecauseofobesityshouldbeconsidered.
-Studyingdiabetescomplications(neuropathy)needtoavoidselectingneuropathy-resistantmousesuchasC57BL/6strain[136].
Stemcellquality-PSCscouldobviatethehurdlesofisletapplicationsuchaslackofdonorsandweaksecretionofinsulinpost-implantation.
-ApplicationofPSCsallowstheunderstandingofpatient-specificdiseasepathogenicityandalsothedevelopmentofpotentialtherapeutics.
-GenerationofiPSCsusingintegrativeorviral-basedmethodshinderstheirclinicalapplicationindiabetestherapy.
-PSCculturesusingundefinedorxenogeneicconditionsproducecellshavingunusualcharacteristicsandpoorphenotypes,andthuscannotbeappliedintheclinic.
-Usingnon-integrativeandsafemethodsforthegenerationofiPSCs.
-DevelopingaccurateassaysforevaluatingthequalityofiPSCs,suchaskaryotyping,analysisofthepluripotencymarkers,andthedifferentiationcapacity.
-Developingefficientmethodsforheterogeneityandteratomaassays.
-Microbiologicalassaysforthedetectionofcellcontamination,suchasmycoplasmatest.
-Usingdefinedandxeno-freecultureconditions.
Organoid/spheroidculture-Organoid/spheroidcultureallowsadetailedunderstandingofdiabetespathogenicity,molecularmechanisms,anddiseasemodelandprovidesausefultoolfordrugscreening.
-Fororganoidculture,Matrigel,collagen-Matrigel,orhydrogelsaremainlyusedasaplatform.
-Applicationofanimal-derivedECMsuchasMatrigelhampersthefurtherapplicationofgeneratedorganoidsintheclinic.
-Organoidcultureiscostlyandlaboriousforthelarge-scaleproduction.
-Designingsuitablesafexenogeneicfreescaffolds(physicalcues)withgrowthfactors(biochemicalcues)forthegenerationofstemcellniche.
-Discoveringacost-effectiveagentsandprotocolsforefficientorganoidcultureatthelargescale.
-Developingefficientassaysfortheevaluationofthegeneratedorganoids/spheroidspriortotheirapplicationfordiseasemodelingordrugscreening.
DifferentiationmethodsVariousdifferentiationprotocolsaredevelopedforthegenerationofinsulin-producingβ-likecellsfromPSCsineithermonolayeror3Dcultureusingacocktailofvariouschemicals,growthfactors,inhibitors,andcytokinesinordertoemulatetheinvivosystem.
-Differentiationprotocolsdependonagentsofhighcosts.
-Manyofthedevelopedprotocolsarenotreproducible.
-Themolecularmechanismsofmostofthechemicalsusedineachstepofthedifferentiationmethodremainunrevealed.
-CharacterizingthereproducibilityofthecurrentβcelldifferentiationprotocolsfromPSCs.
-Settinguphighlyefficientprotocolsforthegenerationofmatureβcellsandtheirtransplantation.
-Cultureconditionssuchasculturemedia,celldensity,ECM,cell-cell,andcell-ECMinteractionshaveanimpactonPSCdifferentiation[68,137–139]andthusshouldbeoptimized.
-Characterizingthemolecularmechanismsofthefactorsusedinthecurrentdifferentiationprotocols.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page14of19Table2Standardcriteriafordesigningandperformingfuturepreclinicalstudiesinvitroandinvivo(Continued)PreclinicaltoolProsCons(challenges)PossibleimprovementsTransplantationdevices-Encapsulationdevicesusedforcelltransplantation,suchassemipermeablecapsuleormembrane,possessvariousfunctions[140]:Avoidingtheundesirablehostimmunereactionsagainstthetransplantedcells.
Protectingthepatientfromtumorigenicactionofstemcells.
Avoidingthelossofviabilityofthetransplantedcells.
Maintainingstableinsulinsecretion-Theencapsulationdevicesneedtheapplicationofimmunemodulatingagents.
-Encapsulationdevicesmayprovokethepatient'simmunesystemandultimatelyleadtocelldeath.
-Applyingsuitableagentswithimmunemodulatingfunctions,summarizedpreviously[140],whichprotectthetransplantedstemcellsfromrejection.
-Designinganefficientencapsulationdevicewiththefollowingfeatures:Allowingenoughbloodsupplytotheencapsulatedcells.
Havingbiocompatibility.
Avoidingthestimulationofhostimmunereactions.
Permittingtheefficienttransferofthesecretedinsulintothecirculation.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page15of19notonlyonthegenerationofmatureβcellsbutalsoontheformationofsubpopulationsofβcellsfromhumanESCs/iPSCsandrevealtheirfunctionalpropertiestopo-tentiallyapplyindiabetes.
ConclusionsTheabilitytoobtainalargenumberofmatureinsulin-producingcellsfromhESC/iPSCcouldprovideun-limitedsuppliesofsurrogateβcellstoreplacedamagedcellsinpatientswithdiabetes.
Insulin-expressingpancreaticcellsgeneratedfromhESC/iPSCtodateappearsimilartoneonatalcells.
Generatingmatureinsulin-expressingcellswiththesameGSIScapabilityasendogenousβcellsandtheirsurvivalfollowingtransplantationintoectopicsitesinexperimentalhostanimalsarechallengesforfuturere-search.
Theprocessesofβcelldifferentiationandisletorga-noidformationarecontrolledbyacomplexnetworkthatdependsontranscriptionalregulationofgenesinvolvedinpancreasdevelopment,acertaintypeandnumberofdiffer-entiationfactors,andspecifictypesandconditionsofstemcellculture.
Althoughmanyfactorsareimportantforthesuccessfulgenerationandtransplantationofinsulin-secret-ingβcellsorislet-likeorganoids,asuitablecombinationoffactorsandconditionsstandsoutasoneofthemostcriticalfactors.
Thus,moreworkisneededtoincreasematurityandpost-transplantsurvivalofhESC/iPSC-derivedinsulin-producingcellsorislet-likeorganoidsthoseresem-bleendogenouspancreaticβcellsorislets,respectively.
Toachievethisgoal,chemicalscreeningofvariousregulatoryfactorsandsmallmoleculesinlatestagesofdifferentiationinvitromaybeagoodoption.
AlistofstandardcriteriafordesigningandperformingfuturepreclinicalstudiesforhPSC-derivedβcells/isletorganoidsinvitroandinvivoisgiveninTable2.
Althoughanumberofconsiderationscur-rentlylimittheuseofhESC/iPSC-derivedcellsincellre-placementtherapies,priorityshouldbegiventotheissuesdiscussedabove.
AbbreviationsBMP:Bonemorphogeneticprotein;DE:Definitiveendoderm;EC:Hormone-expressingendocrinecells;ECCs:Endocrinecellclusters;ECM:Extracellularmatrix;EGF:Epidermalgrowthfactor;EP:Endocrineprogenitor;ERRγ:Estrogen-relatedreceptor-γ;ESC:Embryonicstemcells;FGF:Fibroblastgrowthfactors;GCG+:Glucagon-positivecells;GHRL+:Ghrelin-positivecells;GLP-1:Glucagon-likepeptide-1;GSIS:Glucose-stimulatedinsulinsecretion;HGF:Hepatocytegrowthfactor;HUVEC:Humanumbilicalveinendothelialcell;INS+:Insulin-positivecells;iPSC:Inducedpluripotentstemcells;KGF:Keratinocytegrowthfactor;MEFs:Mouseembryonicfibroblasts;MSCs:Humanmesenchymalstemcells;ND:Non-diabetic;NKX6.
1:NK6homeobox1;NOD:Non-obesediabetes;PDX1:Pancreas/duodenumhomeobox1;PG:Primitiveguttube;PI3K:Phosphatidylinositol-3-kinase;PP:Pancreaticprogenitor;PPY+:Pancreaticpolypeptide-positivecells;PSC:Pluripotentstemcell;SCID:Severecombinedimmunodeficiency;SST+:Somatostatin-positivecells;STZ:Streptozotocin;T1D:Type1diabetes;TGF-β:Transforminggrowthfactor-β;Wnt:WntsignalingAcknowledgementsTheauthorsthankGarrySweeneyforcarefulproofreadingofthetext.
FundingThisworkwassupportedbygrantsfromtheNationalResearchFoundation(NRF)fundedbytheKoreangovernment(2017M3A9C6029562and2015R1A5A1009701).
AvailabilityofdataandmaterialsDatasharingisnotapplicabletothisarticleasnodatasetsweregeneratedoranalyzedduringthecurrentstudy.
Authors'contributionsHMScontributedtotheconception,draft,andmodificationofthemanuscript.
AADcontributedtothedraftandmodificationofthemanuscript.
KMNandTJcontributedtothecollectionandsortingofthedata.
SGCcontributedtothetop-layerdesignandcriticalreviewofthemanuscript.
Allauthorsreadandapprovedthefinalmanuscript.
EthicsapprovalandconsenttoparticipateNotapplicable.
ConsentforpublicationNotapplicable.
CompetinginterestsTheauthorsdeclarethattherearenocompetinginterests.
Publisher'sNoteSpringerNatureremainsneutralwithregardtojurisdictionalclaimsinpublishedmapsandinstitutionalaffiliations.
Authordetails1DepartmentofStemCell&RegenerativeBiotechnologyandIDASI(IncurableDiseaseAnimalmodel&StemcellInstitute),KonkukUniversity,120Neungdong-ro,Gwangjin-gu,Seoul05029,SouthKorea.
2DepartmentofBiochemistryandMolecularBiology,JahangirnagarUniversity,Savar,Dhaka1342,Bangladesh.
References1.
DonathMY,HalbanPA.
Decreasedbeta-cellmassindiabetes:significance,mechanismsandtherapeuticimplications.
Diabetologia.
2004;47:581–9.
2.
RussHA,ParentAV,RinglerJJ,etal.
Controlledinductionofhumanpancreaticprogenitorsproducesfunctionalbeta-likecellsinvitro.
EMBOJ.
2015;34:1759–72.
3.
PosseltAM,SzotGL,FrassettoLA,etal.
Islettransplantationintype1diabeticpatientsusingcalcineurininhibitor-freeimmunosuppressiveprotocolsbasedonT-celladhesionorcostimulationblockade.
Transplantation.
2010;90:1595–601.
4.
BartonFB,RickelsMR,AlejandroR,etal.
Improvementinoutcomesofclinicalislettransplantation:1999–2010.
DiabetesCare.
2012;35:1436–45.
5.
ShapiroAM,RicordiD,HeringBJ,etal.
InternationaltrialoftheEdmontonprotocolforislettransplantation.
NEnglJMed.
2006;355:1318–30.
6.
ShapiroAM.
Stateoftheartofclinicalislettransplantationandnovelprotocolsofimmunosuppression.
CurrDiabRep.
2011;11:345–54.
7.
WhiteSA,ShawJA,SutherlandDE.
Pancreastransplantation.
Lancet.
2009;373:1808–17.
8.
McCALLMD,TosoC,BaetgeEE,etal.
ArestemcellsacurefordiabetesClinSci.
2010;118:87–97.
9.
Dominguez-BendalaJ,InverardiL,RicordiC,etal.
Stemcell-derivedisletcellsfortransplantation.
CurrOpinOrganTransplant.
2011;16:76–82.
10.
D'AmourKA,BangAG,EliazerS,etal.
Productionofpancreatichormone-expressingendocrinecellsfromhumanembryonicstemcells.
NatBiotechnol.
2006;24:1392–401.
11.
JiangW,ShiY,ZhaoD,etal.
Invitroderivationoffunctionalinsulin-producingcellsfromhumanembryonicstemcells.
CellRes.
2007;17:333–44.
12.
ShimJH,KimSE,WooDH,etal.
Directeddifferentiationofhumanembryonicstemcellstowardsapancreaticcellfate.
Diabetologia.
2007;50:1228–38.
13.
EshpeterA,JiangJ,AuM,etal.
Invivocharacterizationoftransplantedhumanembryonicstemcell-derivedpancreaticendocrineisletcells.
CellProlif.
2008;41:843–58.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page16of1914.
KroonE,MartinsonLA,KadoyaK,etal.
Pancreaticendodermderivedfromhumanembryonicstemcellsgeneratesglucose-responsiveinsulin-secretingcellsinvivo.
NatBiotechnol.
2008;26:443–52.
15.
ChenS,BorowiakM,FoxJL,etal.
AsmallmoleculethatdirectsdifferentiationofhumanESCsintothepancreaticlineage.
NatChemBiol.
2009;5:258–65.
16.
ZhangD,JiangW,LiuM,etal.
HighlyefficientdifferentiationofhumanEScellsandiPScellsintomaturepancreaticinsulin-producingcells.
CellRes.
2009;19:429–38.
17.
KunisadaY,Tsubooka-YamazoeN,ShojiM,etal.
Smallmoleculesinduceefficientdifferentiationintoinsulin-producingcellsfromhumaninducedpluripotentstemcells.
StemCellRes.
2012;8:274–84.
18.
RezaniaA,BruinJE,RiedelMJ,etal.
Maturationofhumanembryonicstemcell-derivedpancreaticprogenitorsintofunctionalisletscapableoftreatingpre-existingdiabetesinmice.
Diabetes.
2012;61:2016–29.
19.
SchulzTC,YoungHY,AgulnickAD,etal.
Ascalablesystemforproductionoffunctionalpancreaticprogenitorsfromhumanembryonicstemcells.
PLoSOne.
2012;7:e37004.
20.
BruinJE,RezaniaA,XuJ,etal.
Maturationandfunctionofhumanembryonicstemcell-derivedpancreaticprogenitorsinmacroencapsulationdevicesfollowingtransplantintomice.
Diabetologia.
2013;56:1987–98.
21.
RezaniaA,BruinJE,XuJ,etal.
Enrichmentofhumanembryonicstemcell-derivedNKX6.
1-expressingpancreaticprogenitorcellsacceleratesthematurationofinsulin-secretingcellsinvivo.
StemCells.
2013;31:2432–42.
22.
RezaniaA,BruinJE,AroraP,etal.
Reversalofdiabeteswithinsulin-producingcellsderivedinvitrofromhumanpluripotentstemcells.
NatBiotechnol.
2014;32:1121–33.
23.
PagliucaFW,MillmanJR,GurtlerM,etal.
Generationoffunctionalhumanpancreaticβcellsinvitro.
Cell.
2014;159:428–39.
24.
ShahjalalHM,ShirakiN,SakanoD,etal.
Generationofinsulin-producingbeta-likecellsfromhumaniPScellsinadefinedandcompletelyxeno-freeculturesystem.
JMolCellBiol.
2014;6:394–408.
25.
AgulnickAD,AmbruzsDM,MoormanMA,etal.
Insulin-producingendocrinecellsdifferentiatedinvitrofromhumanembryonicstemcellsfunctioninmacroencapsulationdevicesinvivo.
StemCellsTranslMed.
2015;4:1214–22.
26.
ToyodaT,MaeS-I,TanakaH,etal.
CellaggregationoptimizesthedifferentiationofhumanESCsandiPSCsintopancreaticbud-likeprogenitorcells.
StemCellRes.
2015;14:185–97.
27.
MillmanJR,XieC,DervortAV,etal.
Generationofstemcell-derivedβ-cellsfrompatientswithtype1diabetes.
NatCommun.
2016;7:11463.
28.
ManzarGS,KimEM,ZavazavaN,etal.
Demethylationofinducedpluripotentstemcellsfromtype1diabeticpatientsenhancesdifferentiationintofunctionalpancreaticβ-cells.
JBiolChem.
2017;292:14066–79.
29.
YabeSG,FukudaS,TakedaF,etal.
Efficientgenerationoffunctionalpancreaticβ-cellsfromhumaninducedpluripotentstemcells.
JDiabetes.
2017;9:168–79.
30.
NostroMC,SarangiF,OgawaS,etal.
Stage-specificsignalingthroughTGFβfamilymembersandWNTregulatespatterningandpancreaticspecificationofhumanpluripotentstemcells.
Development.
2011;138:861–71.
31.
XuX,BrowningVL,OdoricoJS.
Activin,BMPandFGFpathwayscooperatetopromoteendodermandpancreaticlineagecelldifferentiationfromhumanembryonicstemcells.
MechDev.
2011;128:412–27.
32.
BruinJE,ErenerS,VelaJ,etal.
Characterizationofpolyhormonalinsulin-producingcellsderivedinvitrofromhumanembryonicstemcells.
StemCellRes.
2014;12:194–208.
33.
BasfordCL,PrenticeKJ,HardyAB,etal.
Thefunctionalandmolecularcharacterisationofhumanembryonicstemcell-derivedinsulin-positivecellscomparedwithadultpancreaticbetacells.
Diabetologia.
2012;55:358–71.
34.
GuoS,DaiC,GuoM,etal.
Inactivationofspecificβcelltranscriptionfactorsintype2diabetes.
JClinInvest.
2013;123:3305–16.
35.
KirkK,HaoE,LahmyR,etal.
Humanembryonicstemcellderivedisletprogenitorsmatureinsideanencapsulationdevicewithoutevidenceofincreasedbiomassorcellescape.
StemCellRes.
2014;12:807–14.
36.
ClinicalTrials.
govIdentifier:NCT02239354.
ViaCyte,Inc.
,SanDiego,CA.
http://viacyte.
com/clinical/clinical-trials.
37.
ThomsonJA,Itskovitz-EldorJ,ShapiroSS,etal.
Embryonicstemcelllinesderivedfromhumanblastocysts.
Science.
1998;282:1145–7.
38.
ReubinoffBE,PeraMF,FongCY,etal.
Embryonicstemcelllinesfromhumanblastocysts:somaticdifferentiationinvitro.
NatBiotechnol.
2000;18:399–404.
39.
CowanCA,KlimanskayaI,McMahonJ,etal.
Derivationofembryonicstem-celllinesfromhumanblastocysts.
NEnglJMed.
2004;350:1353–6.
40.
TakahashiK,YamanakaS.
Inductionofpluripotentstemcellsfrommouseembryonicandadultfibroblastculturesbydefinedfactors.
Cell.
2006;126:663–76.
41.
TakahashiK,TanabeK,OhnukiM,etal.
Inductionofpluripotentstemcellsfromadulthumanfibroblastsbydefinedfactors.
Cell.
2007;131:861–72.
42.
YuJ,VodyanikMA,Smuga-OttoK,etal.
Inducedpluripotentstemcelllinesderivedfromhumansomaticcells.
Science.
2007;318:1917–20.
43.
MaheraliN,HochedlingerK.
Guidelinesandtechniquesforthegenerationofinducedpluripotentstemcells.
CellStemCell.
2008;3:595–605.
44.
FedericoG,BouéS,BelmonteJCI.
Methodsformakinginducedpluripotentstemcells:reprogrammingalacarte.
NatRevGenet.
2011;12:231–42.
45.
O'DohertyR,GreiserU,WangW.
Nonviralmethodsforinducingpluripotencytocells.
BiomedResInt.
2013;2013:705902.
46.
MalikN,RaoMS.
AreviewofthemethodsforhumaniPSCderivation.
MethodsMolBiol.
2013;997:23–33.
47.
ZhouYY,ZengF.
Integration-freemethodsforgeneratinginducedpluripotentstemcells.
GenomicsProteomicsBioinformatics.
2013;11:284–7.
48.
NarayananK,MishraS,SinghS,etal.
Engineeringconceptsinstemcellresearch.
BiotechnolJ.
2017;12:1700066.
49.
MatsuiT,LeungD,MiyashitaH,etal.
ProviralsilencinginembryonicstemcellsrequiresthehistonemethyltransferaseESET.
Nature.
2010;464:927–31.
50.
KimD,KimCH,MoonJI,etal.
Generationofhumaninducedpluripotentstemcellsbydirectdeliveryofreprogrammingproteins.
CellStemCell.
2009;4:472–6.
51.
WoltjenK,MichaelIP,MohseniP,etal.
piggyBactranspositionreprogramsfibroblaststoinducedpluripotentstemcells.
Nature.
2009;458:766–70.
52.
YuJ,HuK,Smuga-OttoK,etal.
Humaninducedpluripotentstemcellsfreeofvectorandtransgenesequences.
Science.
2009;324:797–801.
53.
JiaF,WilsonKD,SunN,etal.
AnonviralminicirclevectorforderivinghumaniPScells.
NatMethods.
2010;7:197–9.
54.
WarrenL,ManosPD,AhfeldtT,etal.
HighlyefficientreprogrammingtopluripotencyanddirecteddifferentiationofhumancellsusingsyntheticmodifiedmRNA.
CellStemCell.
2010;7:618–30.
55.
LeeCH,KimJ-H,LeeHJ,etal.
ThegenerationofiPScellsusingnon-viralmagneticnanoparticlebasedtransfection.
Biomaterials.
2011;32:6683–91.
56.
OkitaK,MatsumuraY,SatoY,etal.
Amoreefficientmethodtogenerateintegration-freehumaniPScells.
NatMethods.
2011;8:409–12.
57.
ChoiHY,LeeT-J,YangG-M,etal.
EfficientmRNAdeliverywithgrapheneoxide-polyethylenimineforgenerationoffootprint-freehumaninducedpluripotentstemcells.
JControlRelease.
2016;235:222–35.
58.
ChinMH,MasonMJ,XieW,etal.
Inducedpluripotentstemcellsandembryonicstemcellsaredistinguishedbygeneexpressionsignatures.
CellStemCell.
2009;5:111–23.
59.
DoiA,ParkIH,WenB,etal.
Differentialmethylationoftissue-andcancer-specificCpGislandshoresdistinguisheshumaninducedpluripotentstemcells,embryonicstemcellsandfibroblasts.
NatGenet.
2009;41:1350–3.
60.
MaysharY,Ben-DavidU,LavonN,etal.
Identificationandclassificationofchromosomalaberrationsinhumaninducedpluripotentstemcells.
CellStemCell.
2010;7:521–31.
61.
PickM,StelzerY,Bar-NurO,etal.
Clone-andgene-specificaberrationsofparentalimprintinginhumaninducedpluripotentstemcells.
StemCells.
2009;27:2686–90.
62.
FengQ,LuSJ,KlimanskayaI,etal.
Hemangioblasticderivativesfromhumaninducedpluripotentstemcellsexhibitlimitedexpansionandearlysenescence.
StemCells.
2010;28:704–12.
63.
HuB-Y,WeickJP,YuJ,etal.
Neuraldifferentiationofhumaninducedpluripotentstemcellsfollowsdevelopmentalprinciplesbutwithvariablepotency.
ProcNatlAcadSci.
2010;107:4335–40.
64.
UrbachA,Bar-NurO,DaleyGQ,etal.
DifferentialmodelingoffragileXsyndromebyhumanembryonicstemcellsandinducedpluripotentstemcells.
CellStemCell.
2010;6:407–11.
65.
MiuraK,OkadaY,AoiT,etal.
Variationinthesafetyofinducedpluripotentstemcelllines.
NatBiotechnol.
2009;27:743–5.
66.
AssadyS,MaorG,AmitM,etal.
Insulinproductionbyhumanembryonicstemcells.
Diabetes.
2001;50:1691–7.
67.
Aguayo-MazzucatoC,ZavackiAM,MarinelarenaA,etal.
Thyroidhormonepromotespostnatalratpancreaticβ-celldevelopmentandglucose-responsiveinsulinsecretionthroughMAFA.
Diabetes.
2013;62:1569–80.
68.
MemonB,KaramM,Al-KhawagaS,etal.
Enhanceddifferentiationofhumanpluripotentstemcellsintopancreaticprogenitorsco-expressingPDX1andNKX6.
1.
StemCellResTher.
2018;9:15.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page17of1969.
NostroMC,SarangiF,YangC,etal.
EfficientgenerationofNKX6-1+pancreaticprogenitorsfrommultiplehumanpluripotentstemcelllines.
StemCellRep.
2015;4:591–604.
70.
deKrijgerRR,AanstootHJ,KranenburgG,etal.
Themidgestationalhumanfetalpancreascontainscellscoexpressingislethormones.
DevBiol.
1992;153:368–75.
71.
HrvatinS,O'DonnellCW,DengF,etal.
Differentiatedhumanstemcellsresemblefetal,notadult,βcells.
ProcNatlAcadSci.
2014;111:3038–43.
72.
RiedelMJ,AsadiA,WangR,etal.
Immunohistochemicalcharacterisationofcellsco-producinginsulinandglucagoninthedevelopinghumanpancreas.
Diabetologia.
2012;55:372–81.
73.
KellyOG,ChanMY,MartinsonLA,etal.
Cell-surfacemarkersfortheisolationofpancreaticcelltypesderivedfromhumanembryonicstemcells.
NatBiotechnol.
2011;29:750–6.
74.
XieR,EverettLJ,LimH-W,etal.
Dynamicchromatinremodelingmediatedbypolycombproteinsorchestratespancreaticdifferentiationofhumanembryonicstemcells.
CellStemCell.
2013;12:224–37.
75.
RojasA,KhooA,TejedoJR,etal.
Isletcelldevelopment.
AdvExpMedBiol.
2010;654:59–75.
76.
SeymourPA,SanderM.
Historicalperspective:beginningsoftheβ-cell:currentperspectivesinβ-celldevelopment.
Diabetes.
2011;60:364–76.
77.
ArdaHE,BenitezCM,KimSK,etal.
Generegulatorynetworksgoverningpancreasdevelopment.
DevCell.
2013;25:5–13.
78.
RorsmanP,BraunM.
Regulationofinsulinsecretioninhumanpancreaticislets.
AnnuRevPhysiol.
2013;75:155–79.
79.
BenningerRKP,PistonDW.
Cellularcommunicationandheterogeneityinpancreaticisletinsulinsecretiondynamics.
TrendsEndocrinolMetab.
2014;25:399–406.
80.
PeirisH,BonderCS,CoatesPT,etal.
Theβ-cell/ECaxis:howdoisletcellstalktoeachotherDiabetes.
2014;63:3–11.
81.
WangW,JinS,YeK,etal.
DevelopmentofisletorganoidsfromH9humanembryonicstemcellsinbiomimetic3Dscaffolds.
StemCellsDev.
2017;26:394–404.
82.
CandielloJ,PavanGrandhiTS,GohSK,etal.
3Dheterogeneousisletorganoidgenerationfromhumanembryonicstemcellsusinganovelengineeredhydrogelplatform.
Biomaterials.
2018;177:27–39.
83.
JiangJ,AuM,LuK,etal.
Generationofinsulin-producingislet-likeclustersfromhumanembryonicstemcells.
StemCells.
2007;25:1940–53.
84.
TateishiK,HeJ,TaranovaO,etal.
Generationofinsulin-secretingislet-likeclustersfromhumanskinfibroblasts.
JBiolChem.
2008;283:31601–7.
85.
ShimJH,KimJ,HanJ,etal.
Pancreaticislet-likethree-dimensionalaggregatesderivedfromhumanembryonicstemcellsamelioratehyperglycemiainstreptozotocin-induceddiabeticmice.
CellTransplant.
2015;24:2155–68.
86.
KimY,KimH,KoUH,etal.
Islet-likeorganoidsderivedfromhumanpluripotentstemcellsefficientlyfunctionintheglucoseresponsivenessinvitroandinvivo.
SciRep.
2016;6:35145.
87.
TakahashiY,SekineK,KinT,etal.
Self-condensationcultureenablesvascularizationoftissuefragmentsforefficienttherapeutictransplantation.
CellRep.
2018;23:1620–9.
88.
HickmanGJ,BoocockDJ,PockleyAG,etal.
Theimportanceandclinicalrelevanceofsurfacesintissueculture.
ACSBiomaterSciEng.
2016;2:152–64.
89.
WaltersNJ,GentlemanE.
Evolvinginsightsincell-matrixinteractions:elucidatinghownon-solublepropertiesoftheextracellularnichedirectstemcellfate.
ActaBiomater.
2015;11:3–16.
90.
BakerLA,TiriacH,CleversH,etal.
Modelingpancreaticcancerwithorganoids.
TrendsCancer.
2016;2:176–90.
91.
YinX,MeadBE,SafaeeH,etal.
Engineeringstemcellorganoids.
CellStemCell.
2016;18:25–38.
92.
GieniRS,HendzelMJ.
MechanotransductionfromtheECMtothegenome:arethepiecesnowinplaceJCellBiochem.
2008;104:1964–87.
93.
ThomasD,O'BrienT,PanditA.
Towardcustomizedextracellularnicheengineering:progressincell-entrapmenttechnologies.
AdvMater.
2018;30:1703948.
94.
SchuppinGT,Bonner-WeirS,MontanaE,etal.
Replicationofadultpancreatic-betacellsculturedonbovinecornealendothelialcellextracellularmatrix.
InVitroCellDevBiolAnim.
1993;29A:339–44.
95.
BoscoD,MedaP,HalbanPA,etal.
Importanceofcell-matrixinteractionsinratisletbeta-cellsecretioninvitro:roleofalpha6beta1integrin.
Diabetes.
2000;49:233–43.
96.
WeberLM,HaydaKN,AnsethKS,etal.
Cell-matrixinteractionsimprovebeta-cellsurvivalandinsulinsecretioninthree-dimensionalculture.
TissueEngPartA.
2008;14:1959–68.
97.
RisF,HammarE,BoscoD,etal.
Impactofintegrin-matrixmatchingandinhibitionofapoptosisonthesurvivalofpurifiedhumanbeta-cellsinvitro.
Diabetologia.
2002;45:841–50.
98.
HammarE,ParnaudG,BoscoD,etal.
Extracellularmatrixprotectspancreaticβ-cellsagainstapoptosis:roleofshort-andlong-termsignalingpathways.
Diabetes.
2004;53:2034–41.
99.
LeeJH,YuHS,LeeGS,etal.
Collagengelthree-dimensionalmatricescombinedwithadhesiveproteinsstimulateneuronaldifferentiationofmesenchymalstemcells.
JRSocInterface.
2011;8:998–1010.
100.
ZimmermannWH,SchneiderbangerK,SchubertP,etal.
Tissueengineeringofadifferentiatedcardiacmuscleconstruct.
CircRes.
2002;90:223–30.
101.
LuS-H,WangH-B,LiuH,etal.
Reconstructionofengineereduterinetissuescontainingsmoothmusclelayerincollagen/Matrigelscaffoldinvitro.
TissueEngPartA.
2009;15:1611–8.
102.
LiW,ZhaoR,LiuJ,etal.
Smallisletstransplantationsuperioritytolargeones:implicationsfromisletmicrocirculationandrevascularization.
JDiabetesRes.
2014;2014:192093.
103.
TakebeT,EnomuraM,YoshizawaE,etal.
Vascularizedandcomplexorganbudsfromdiversetissuesviamesenchymalcell-drivencondensation.
CellStemCell.
2015;16:556–65.
104.
LancasterMA,KnoblichJA.
Organogenesisinadish:modelingdevelopmentanddiseaseusingorganoidtechnologies.
Science.
2014;345:1247125.
105.
TakahashiY,TakebeT,TaniguchiH,etal.
Engineeringpancreatictissuesfromstemcellstowardstherapy.
RegenTher.
2016;3:15–23.
106.
YanagawaF,KajiH,JangY-H,etal.
Directedassemblyofcell-ladenmicrogelsforbuildingporousthree-dimensionaltissueconstructs.
JBiomedMaterResA.
2011;97:93–102.
107.
KharkarPM,KiickKL,KloxinAM.
Designingdegradablehydrogelsfororthogonalcontrolofcellmicroenvironments.
ChemSocRev.
2013;42:7335–72.
108.
StendahlJC,KaufmanDB,StuppSI.
Extracellularmatrixinpancreaticislets:relevancetoscaffolddesignandtransplantation.
CellTransplant.
2009;18:1–12.
109.
DudleyAC.
Tumorendothelialcells.
ColdSpringHarbPerspectMed.
2012;2:a006536.
110.
KreutzigerKL,MuskheliV,JohnsonP,etal.
Developingvasculatureandstromainengineeredhumanmyocardium.
TissueEngPartA.
2011;17:1219–28.
111.
OkitaK,IchisakaT,YamanakaS.
Generationofgermline-competentinducedpluripotentstemcells.
Nature.
2007;448:313–7.
112.
NakagawaM,KoyanagiM,TanabeK,etal.
GenerationofinducedpluripotentstemcellswithoutMycfrommouseandhumanfibroblasts.
NatBiotechnol.
2008;26:101–6.
113.
Hacein-Bey-AbinaS,VonKalleC,SchmidtM,etal.
LMO2-associatedclonalTcellproliferationintwopatientsaftergenetherapyforSCID-X1.
Science.
2003;302:415–9.
114.
StadtfeldM,NagayaM,UtikalJ,etal.
Inducedpluripotentstemcellsgeneratedwithoutviralintegration.
Science.
2008;322:945–9.
115.
ZhouW,FreedCR.
Adenoviralgenedeliverycanreprogramhumanfibroblaststoinducedpluripotentstemcells.
StemCells.
2009;27:2667–74.
116.
FusakiN,BanH,NishiyamaA,etal.
Efficientinductionoftransgene-freehumanpluripotentstemcellsusingavectorbasedonSendaivirus,anRNAvirusthatdoesnotintegrateintothehostgenome.
ProcJapanAcadSerB.
2009;85:348–62.
117.
OkitaK,YamanakaS.
Inductionofpluripotencybydefinedfactors.
ExpCellRes.
2010;316:2565–70.
118.
OsafuneK,CaronL,BorowiakM,etal.
Markeddifferencesindifferentiationpropensityamonghumanembryonicstemcelllines.
NatBiotechnol.
2008;26:313–5.
119.
CoboF,StaceyG,HuntC,etal.
Microbiologicalcontrolinstemcellbanks:approachestostandardisation.
ApplMicrobiolBiotechnol.
2005;68:456–66.
120.
MartinMJ,MuotriA,GageF,etal.
Humanembryonicstemcellsexpressanimmunogenicnonhumansialicacid.
NatMed.
2005;11:228–32.
121.
SkottmanH,HovattaO.
Cultureconditionsforhumanembryonicstemcells.
Reproduction.
2006;132:691–8.
122.
MicallefSJ,LiX,SchiesserJV,etal.
INSGFP/whumanembryonicstemcellsfacilitateisolationofinvitroderivedinsulin-producingcells.
Diabetologia.
2012;55:694–706.
123.
YoshiharaE,WeiZ,LinCS,etal.
ERRγisrequiredforthemetabolicmaturationoftherapeuticallyfunctionalglucose-responsiveβcells.
CellMetab.
2016;23:622–34.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page18of19124.
SaberN,BruinJE,O'DwyerS,etal.
Sexdifferencesinmaturationofhumanembryonicstemcell-derivedβcellsinmice.
Endocrinology.
2018;159:1827–41.
125.
SchuitF,VanLommelL,GranvikM,etal.
β-cell–specificgenerepression:amechanismtoprotectagainstinappropriateormaladjustedinsulinsecretionDiabetes.
2012;61:969–75.
126.
PepperAR,Gala-LopezB,PawlickR,etal.
Aprevascularizedsubcutaneousdevice-lesssiteforisletandcellulartransplantation.
NatBiotechnol.
2015;33:518–23.
127.
VegasAJ,VeisehO,GurtlerM,etal.
Long-termglycemiccontrolusingpolymerencapsulatedhumanstem-cellderivedβ-cellsinimmunecompetentmice.
NatMed.
2016;22:306–11.
128.
WeirGC.
Isletencapsulation:advancesandobstacles.
Diabetologia.
2013;56:1458–61.
129.
HermannM,PirkebnerD,DraxlA,etal.
Dickkopf-3isexpressedinasubsetofadulthumanpancreaticbetacells.
HistochemCellBiol.
2007;127:513–21.
130.
SaishoY,HarrisPE,ButlerAE,etal.
Relationshipbetweenpancreaticvesicularmonoaminetransporter2(VMAT2)andinsulinexpressioninhumanpancreas.
JMolHistol.
2008;39:543–51.
131.
DorrellC,SchugJ,CanadayPS,etal.
Humanisletscontainfourdistinctsubtypesofβcells.
NatCommun.
2016;7:11756.
132.
WallisRH,WangK,MarandiL,etal.
Type1diabetesintheBBrat:apolygenicdisease.
Diabetes.
2009;58:1007–17.
133.
ZhangW,KamiyaH,EkbergK,etal.
C-peptideimprovesneuropathyintype1diabeticBB/Wor-rats.
DiabetesMetabResRev.
2007;23:63–70.
134.
vonHerrathM,FilippiC,CoppietersK.
Howviralinfectionsenhanceorpreventtype1diabetes-frommousetoman.
JMedVirol.
2011;83:1672.
135.
MullerYD,GolshayanD,EhirchiouD,etal.
Immunosuppressiveeffectsofstreptozotocin-induceddiabetesresultinabsolutelymphopeniaandarelativeincreaseofT-regulatorycells.
Diabetes.
2011;60:2331–40.
136.
BrosiusFC,AlpersCE,BottingerEP,etal.
Mousemodelsofdiabeticnephropathy.
JAmSocNephrol.
2009;20:2503–12.
137.
GageBK,WebberTD,KiefferTJ.
Initialcellseedingdensityinfluencespancreaticendocrinedevelopmentduringinvitrodifferentiationofhumanembryonicstemcells.
PLoSOne.
2013;8:e82076.
138.
RazaA,ChangSK,LinCC.
Theinfluenceofmatrixpropertiesongrowthandmorphogenesisofhumanpancreaticductalepithelialcellsin3D.
Biomaterials.
2013;34:5117–27.
139.
ShihHP,PanlasiguiD,CirulliV,etal.
ECMsignalingregulatescollectivecellulardynamicstocontrolpancreasbranchingmorphogenesis.
CellRep.
2016;14:169–79.
140.
SneddonJB,TangQ,StockP,etal.
Stemcelltherapiesfortreatingdiabetes:progressandremainingchallenges.
CellStemCell.
2018;22:810–23.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page19of19
Shahjalal1,2,AhmedAbdalDayem1,KyungMinLim1,Tak-ilJeon1andSsang-GooCho1*AbstractHumanembryonicstemcells(hESC)andinducedpluripotentstemcells(hiPSC)areconsideredattractivesourcesofpancreaticβcellsandisletorganoids.
Recently,severalreportspresentedthathESC/iPSC-derivedcellsenrichedwithspecifictranscriptionfactorscanformglucose-responsiveinsulin-secretingcellsinvitroandtransplantationofthesecellsameliorateshyperglycemiaindiabeticmice.
However,theglucose-stimulatedinsulin-secretingcapacityofthesecellsislowerthanthatofendogenousislets,suggestingtheneedtoimproveinductionprocedures.
OneofthecriticalproblemsfacinginvivomaturationofhESC/iPSC-derivedcellsistheirlowsurvivalrateaftertransplantation,althoughthisrateincreaseswhentheimplantedpancreaticcellsareencapsulatedtoavoidtheimmuneresponse.
SeveralgroupshavealsoreportedonthegenerationofhESC/iPSC-derivedislet-likeorganoids,butdevelopmentoftechniquesforcompleteisletstructureswiththeeventualgenerationofvascularizedconstructsremainsamajorchallengetotheirapplicationinregenerativetherapies.
ManyissuesalsoneedtobeaddressedbeforethesuccessfulclinicalapplicationofhESC/iPSC-derivedcellsorisletorganoids.
Inthisreview,wesummarizeadvancesinthegenerationofhESC/iPSC-derivedpancreaticβcellsorisletorganoidsanddiscussthelimitationsandchallengesfortheirsuccessfultherapeuticapplicationindiabetes.
Keywords:Embryonicstemcells(ESC),Inducedpluripotentstemcells(iPSC),Differentiation,Pancreaticβcell,Isletorganoids,Transplantation,βCellmaturationBackgroundDiabetesmellitusisalife-threateningdisease,anditsprevalenceisincreasingworldwide.
Theavailabletreat-mentcanneithercurenorcompletelycontrolthecom-plicationsofthisdisorder,whichresultsinsubstantiallossesoflifeinalmostallcountriesintheworld.
Fur-thermore,currentlife-longtreatmentstrategiesimposelargesocialandeconomicburdensonafamily.
Forthelastfewdecades,humanbeingshavebeentryingtode-velopatreatmentstrategythatcaneffectivelycontrolthisdisorderandsavelives.
Despitetremendousefforts,however,humanshavebeenfarfromsuccessinfindinganeffectivetreatmentstrategyfordiabetes.
Type1diabetesresultsfromanabsolutedeficiencyofinsulinduetoTcell-mediatedautoimmunedestructionofpancreasβcells[1].
Thecurrenttreatmentfortype1diabetesissolelydependentontheadministrationofex-ogenousinsulin.
Althoughthisapproachmanagesthedisease,unwantedrisksandlong-termcomplicationspersistbecauseoftheinabilitytotightlymaintainglucoselevelswithinanormalphysiologicalrange.
Complicationsincludelife-threateningepisodesofhypoglycemia,aswellaslong-termcomplicationsthatincludemicro-andmacro-angiopathyleadingtocardio-vascularpathologies,kidneyfailure,andneuropathy.
Thus,thereisaneedfornewtreatmentsthatprovidesuperiorcontrolofbloodglucosetominimizethesecomplications[2].
Oneexistingapproachtotreatingdia-betesistransplantationofpurifiedhumancadavericis-letsintotheportalveintoreplacethedestroyedβcellsofthepatients.
Thisproceduretypicallyresultsinbetterglycemiccontrol,canrenderpatientsinsulinindepend-entforprolongedperiodsoftime,andimprovesoverall*Correspondence:ssangoo@konkuk.
ac.
kr;ssangoo33@gmail.
comHussainMd.
ShahjalalandAhmedAbdalDayemcontributedequallytothiswork.
1DepartmentofStemCell&RegenerativeBiotechnologyandIDASI(IncurableDiseaseAnimalmodel&StemcellInstitute),KonkukUniversity,120Neungdong-ro,Gwangjin-gu,Seoul05029,SouthKoreaFulllistofauthorinformationisavailableattheendofthearticleTheAuthor(s).
2018OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355https://doi.
org/10.
1186/s13287-018-1099-3qualityoflife[3,4].
Althoughpromising,becauseofdif-ficultiessuchasthescarcityofcadavericdonorscom-paredtothelargenumberofdiabeticpatients,lowyieldoftransplantableisletsfromcadavericpancreases,andnecessityforchronicimmunosuppressiontopreventre-jectionoftheallograft[5,6],analternativesourceofsurrogatecellsisneeded.
Moreover,thenumberoffunc-tionalβcellsthatcanbeextractedfromasinglecadav-ericpancreasisoftennotenoughtorestoreeuglycemiainasinglediabeticpatient[7].
Thisalsoillustratestheneedforalternativesourcesofβcellstotreatthein-creasingnumberofdiabeticpatients.
Humanpluripotentstemcells(hPSCs),includinghu-manembryonicstemcells(hESC)andinducedpluripo-tentstemcells(hiPSC),areconsideredveryattractivealternativesourcesofsurrogateβcellsbecauseoftheirabilitytodifferentiateintoallmajorsomaticcelllineages[8,9].
Todate,themostsuccessinproducingpancreaticβ-likecellsfromhPSCshascomefromapproachesthatmimicnormalpancreasdevelopment.
Manyresearchgroupshavefollowedthisapproach,whichinvolvesex-posingthecellstovariousgrowthfactorsandsignalingmoleculesatspecificdosesandinaparticularsequencetosuccessfullydifferentiatethecellsintopancreaticendodermorendocrinecells(ECs)[2,10–29].
However,inmanystudies,alargenumberofpolyhormonalinsulin-expressingcellshavebeenobservedinculturethatresembletransientECsseeninmid-gestationhu-manfetalpancreases[10,11,15–17,30–32].
Thesepoly-hormonalcellslackexpressionofkeyβcelltranscriptionfactorsanddonotsecreteinsulininvitroinresponsetoglucosechallenge—thehallmarkfunctionofbonafideβcells[10,32–34](Fig.
1a).
Concurrently,inseveralotherstudies,analternativestrategyhasbeenadoptedinwhichglucose-responsiveinsulin-secretingcellscanbegeneratedfollowingtransplantationofhESC/iPSC-derivedpancreaticprogenitorcellsintoectopicsitesinimmuno-deficientortype1diabeticmice[12,14,18–21,26].
Inre-cipientmice,theresultingcellscanproducehumaninsulintoreversediabetes[18,20,21](Fig.
1b).
Inrecentyears,optimizeddifferentiationprotocolshavebeensuc-cessfullydevelopedtogenerateglucose-responsiveinsulin-secretingcellsinvitrofromhESC/iPSC,whichex-pressmatureβcellmarkers,andtransplantationoftheseabcFig.
1Differentiation,maturation,andfunctionofpancreaticβcellsderivedfromhESC/iPSC.
Insulin-positivepolyhormonalcellsmostlyformedinmanyinvitrocellcultureprotocolswhichshowlimitedornoGSIS(a).
Alternatively,EPcellswereformedfromhESC/iPSCinamonolayerand/orrotatingsuspensionculture,andtransplantationofthesecellsgeneratedislet-likeECsthatexhibitedGSISandcouldreversehyperglycemia(b).
Recently,pancreaticβ-likecellsexpressingmatureβcellmarkersandexhibitingGSISinvitroweregeneratedineitherlowadhesioncultureorrotatingsuspensionculture;aftertransplantation,thesecellsunderwentfurthermaturation,secretedinsulininresponsetoglucose,andamelioratedhyperglycemiaindiabeticmice(c).
GSIS,glucose-stimulatedinsulinsecretion;AFP,hepaticprogenitorcellsexpressingAFP;CDX2,intestinalprogenitorcellsexpressingCDX2;PP,pancreaticprogenitor;EP,endocrineprecursor;INS,β-likecellsexpressinginsulin;GCG,αcellsexpressingglucagon;SST,δcellsexpressingsomatostatinShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page2of19cellshasbeenshowntoamelioratehyperglycemiaindia-beticmice[2,22,23,29](Fig.
1c).
Theβ-likecellsgener-atedshowgeneexpression,ultrastructuralcharacteristics,andglucoseresponsivenessbothinvitroandinvivo,whichcloselyresemblingthefeaturesofβcellsfoundinpancreaticislets[2,22,23].
Inthesemultistageprotocols,thefinalcellpopulationhasabout30–60%β-likecells,andthemajorityoftheremainingcellsarerelativelyuncharacterizedcellsthatcanbeundifferentiatedprogeni-torsorothertypesofunwantedcells.
Thus,improvingef-ficiency,intermsofthepercentageofdifferentiatedcellsthatbecomeβcells,remainsanimportantchallenge.
Althoughtremendoussuccesshasbeenachievedinthelastfewyears,lowsurvivalratesofhESC/iPSC-der-ivedpancreaticcellsaftertransplantationintoectopicsitesinrecipientsremainacriticalproblem[20,25,35].
Therefore,anefficientculturesystemthatcanbeusedtogeneratefunctionalandterminallydifferentiatedβcells,alongwithaneffectivetransplantationtechnique,isneededforclinicalapplicationofhESC/iPSC-derivedβcellsfordiabetestreatment.
However,phase1/2clin-icaltrialsfortheapplicationofhESC-derivedpancreaticprogenitorsintype1diabetespatientshavealreadybegun[36].
Inthisreview,wesummarizeadvancesinthedifferentiationofhESC/iPSC-derivedcellsintopan-creaticβcellsandislet-likeorganoidsanddiscussthelimitationsandchallengesfortheirsuccessfulgenerationandtherapeuticapplicationintype1diabetes.
PluripotentstemcellsandtheirreprogrammingESCsshowunlimitedreplicativepropertiesandthepo-tentialtodifferentiateintoanyadultcelltype[37–39].
iPSCs,establishedfromsomaticcellsofmouseandhu-man[40–42],havethesameabilitytoexpandanddiffer-entiateasESCs.
Therefore,bothESCsandiPSCshavegreatpotentialforuseincelltherapies.
However,theuseofiPSCshasfewerethicalcomplicationsthanESCsthatarederivedfromtheinnercellmassoflivingembryos.
iPSCsarederivedfromvarioussomaticcellsafterexpos-uretoacombinationoftranscriptionfactorssuchasOct3/4,Sox2,Klf4,andc-Myc[40,41].
iPSCgenerationiscarriedoutviaviral-basedandnon-viral-basedmethodsassummarizedinFig.
2.
Thesemethodsarevariedintheirefficiencies,transductionperiod,genomeFig.
2GenerationofiPSCsfromvarioussomaticcells.
iPSCgenerationcarriedoutviaviral-basedandnon-viral-basedmethodsaresummarizedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page3of19integration,andcost[43–48].
Therefore,selectionofthereprogrammingmethoddeterminesthefurtherapplica-tionoftheproducediPSCinregenerativemedicine.
Generally,viral-basedmethodsleadtogenomeintegra-tionandareoflowsafety,albeit,thehighefficiency.
MostiPSCsaremadeusingretrovirusvectors,whichin-tegratereprogrammingfactorsintohostgenomes.
Retrovirusvectorscanspontaneouslyinfectvariouscelltypesandinserttheircodinggenesintohostgenomesusingreversetranscriptase,whichallowscontinuoustransgeneexpressionduringreprogramming.
RetroviraltransgeneexpressioncontinuesuntilthecellsbecomeiPSCs,andthen,theretroviralpromoterisinactivated,possiblybecauseofepigeneticmodificationssuchashis-tonemethylation[49].
Thisguidedreprogrammingandautomaticsilencingmechanismisconsideredveryim-portantforiPSCinductionfromsomaticcells.
Recently,severalvirus-freetechniqueshavebeendevelopedfortheproductionoffootprint-freeiPSCs;theirefficientculturetechniqueshavealsobeenestablished[50–57].
ESCsvs.
iPSCs:similaritiesanddifferencesSimilartoESCs,iPSCshaveacharacteristicmorphology,abilitytogenerateembryoidbodiesandteratomas,andunlimitedproliferationcapabilityinvitro,whiletheymaintaintheirpluripotencybyexpressingpluripotencygenes.
However,severalstudieshaverevealedsomedif-ferencesbetweenhESCsandhiPSCsintermsofgeneex-pressionprofiles[58],epigeneticmodificationssuchasDNAmethylation[59],geneticstability[60],imprintedgeneexpressionstability[61],differentiationpotentials[62,63],anddiseasemodeling[64].
iPSCshavesome"memory"oftheirsomaticoriginandthereforearenotidenticaltoESCs.
ThememoryofiPSCmayaffecttheirsafety[65].
However,thereisnosufficientevidenceyettodeterminewhetheriPSCmemorycanbefatalincelltherapies.
DifferentiationofhESC/iPSCintopancreaticβcellsInsulin-producingcellswithpancreaticβcellcharacter-isticswerefirstsuccessfullyderivedinembryoidbodiesfromspontaneousdifferentiationofhESC[66].
Sincethen,numerousmethodstogeneratepancreaticendo-dermorβ-likecellsfromhESC/iPSChavebeenreported[2,10–29].
Thesestudiesdemonstratedthegenerationofinsulin-positivecells,aswellasglucagon-andsomatostatin-positivecells(Table1).
However,theper-centagesofinsulin-positivecellsobtainedinculturevaryamongtheprotocols.
Thekeystagesofembryonicpancreasdevelopmentin-cludedevelopmentofthedefinitiveendoderm(DE),primitiveguttube(PG),pancreaticprogenitor(PP),endo-crineprogenitor(EP),andhormone-expressingECs.
Basedoninformationaboutembryonicpancreasdevelop-ment,eachdifferentiationprotocolhasbeendesignedtousevariouscytokinesorsignalingmodulatorsatspecificdosesandinparticularsequencestoactivateorinhibitkeysignalingpathways,includingnodal/activin,Wnt,PI3K,fibroblastgrowthfactors(FGF),bonemorphogeneticpro-tein(BMP),retinoicacid,hedgehog,proteinkinaseC,notch,epidermalgrowthfactor,andtransforminggrowthfactor-β(TGF-β).
Othergrowthfactorssuchasinsulin-likegrowthfactors1and2,hepatocytegrowthfac-tor(HGF),andglucagon-likepeptide-1(GLP-1)orexendin-4(apeptideanalogofGLP-1)havealsobeenusedtofacilitatedifferentiationofpancreatichormone-ex-pressingcells[10,11,13,15,16,24].
Inaddition,variousclassesofsmallmoleculeshavebeenreportedtobeeffect-ivefordifferentiationofhESC/iPSCintoinsulin-produ-cingcells.
Nicotinamide,apoly(ADP-ribose)synthetaseinhibitor,isusedinsomeprotocolstoimprovetheyieldofpancreaticECs[11,13,16,17,24].
Further,forskolin(anactivatorofadenylylcyclase)anddexamethasone(asyn-theticadrenocorticalsteroid)havebeenshowntoenhancecellularmaturation,andtheseagentscanbecombinedwithothersmallmoleculestoobtainsynergisticeffects[17].
Thyroidhormonepromotespostnatalβcelldevelop-mentandglucose-responsiveinsulinsecretioninratsthroughthetranscriptionfactorMAFA[67].
Thisinsighthasincreasedtheuseofthyroidhormoneinrecentproto-colstoimproveglucoseresponsivenessofhESC/iPSC-der-ivedβcells[22,23,25,27,28,68].
Severalreportshaverecognizedpancreaticprogenitorsco-expressingPancre-aticandDuodenalHomeobox1(PDX1)andNK6homeo-box1(NKX6.
1)asindispensableprecursorsofmaturepancreaticβcells[18,21,26].
Differentiationintopancre-aticprogenitorsco-expressingPDX1andNKX6.
1canbeenhancedinvitrobyeitherdissociatingdenselyformedendodermalcellsandre-platingthesecellsatalowdensityfollowedbyexposuretoalongerperiodofretinoidandFGF10signaling[68]orcultureswithhigh-densityag-gregates[26]orrotatingasuspensioncultureaftertheadditionoffactorssuchasALK5i(aTGF-βtypeIreceptorkinaseinhibitorII),TBP(aPKCactivator),and/orLDN(aBMPinhibitor)[18,21,23].
Theuseofepidermalgrowthfactor(EGF)andnicotinamideinthepancreaticprogenitorspecificationstagecanalsosignifi-cantlyenhancepancreaticprogenitorco-expressingPDX1andNKX6.
1[69].
MaturationofhESC/iPSC-derivedβcellsThematurationofpancreaticβ-likecellsobtainedbydifferentiationfromhESC/iPSCinvitroremainscontro-versial.
Intheearlystudies,eitherMatrigelorlow-densitymouseembryonicfibroblast(MEF)wasusedasa2DcultureplatformonwhichhESC/iPSCwereseeded[10,11,15–17,30–32].
TheseprotocolsShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page4of19Table1Generationofinsulin-positiveβ-likecellsfromhESC/iPSC,theirmaturation,andfunctionsinvitroandinvivoReferences[Celllinesused]DifferentiationconditionCelltypesinducedPercentinsulin+cellsGSISRecipients/transplantationsiteAmeliorationofhyperglycemiaD'Amouretal.
[10]CyT203[hESCline]Onlow-densityMEFsINS+,GCG+,SST+,PPY+,GHRL+7.
3%(3–12%)Non.
a.
n.
d.
Jiangetal.
[11]H1,H9[hESCline]OnMatrigelINS+,GCG+,SST+[n.
t:PPY+,GHRL+]>15%Yes(invitro)BALB/cnudemice/kidneycapsuleYesShimetal.
[12]Miz-hES4,Miz-hES6[hESCline]SuspensioncultureINS+,GCG+,SST+n.
d.
n.
d.
BALB/cnudemice/kidneycapsuleYesEshpeteretal.
[13]H1[hESCline]OnMatrigelINS+,GCG+,SST+5.
3%Yes(invivo)DiabeticC57BL6Rag1/1mice/kidneycapsuleNoKroonetal.
[14]CyT49,CyT203[hESCline]Onlow-densityMEFsINS+,GCG+,SST+,PPY+,GHRL+n.
d.
Yes(invivo)SCID-beigemice/epididymalfatpadYesChenetal.
[15]HUES-2,HUES-4,HUES-8,HUES-9[hESCline]Onlow-densityMEFsINS+,GCG+,SST+,[n.
t:PPY+,GHRL+]0.
8±0.
4%Low(invitro)CD1nudemice/kidneycapsulen.
d.
Zhangetal.
[16]H1,H9[hESCline];C1,C2,C5[hiPSCline]OnMatrigelINS+,SST+25%Yes(invitro)n.
a.
n.
d.
Kunisadaetal.
[17]253G1,201B7,297A1,297F1,and297L1[hiPSCline]Onlow-densityMEFsINS+,GCG+,SST+,GHRL+11.
8%(8.
0–16.
9%)Non.
a.
n.
d.
Rezaniaetal.
[18]H1,ESI-49[hESCline]Matrigel/suspensionculture(stirred)INS+,GCG+,SST+,PPY+~10%Yes(invivo)SCID-beigeandSTZ-diabeticmice/kidneycapsuleYesSchulzetal.
[19]CyT49[hESCline]Suspension(aggregates)INS+,GCG+,SST+,[n.
t:PPY+,GHRL+]n.
d.
Yes(invivo)SCID-beigemice/epididymalfatpadYesRezaniaetal.
[21]H1[hESCline]Matrigel/suspensionculture(stirred)INS+,GCG+,SST+,PPY+,GHRL+~55–60%(post-transplant)Yes(invivo)SCID-beigeandSTZ-diabeticmice/subcutaneouswithencapsulationdeviceYesBruinetal.
[20]H1[hESCline]Matrigel/suspensionculture(stirred)INS+,GCG+,SST+n.
d.
Yes(invivo)SCID-beigeandSTZ-diabeticmice/kidneycapsuleandsubcutaneouswithencapsulationdeviceYesShahjalaletal.
[24]Toe,201B7[hiPSC];KhES-3[hESCline]OnSynthemax(xeno-free)INS+,GCG+,SST+5–8%Yes(invitro)n.
a.
n.
d.
Rezaniaetal.
[22]H1[hESCline];anepisomalhiPSCPlanarculture/air-liquidinterfacecultureINS+,GCG+,SST+~50%Yes(invitroandinvivo)Non-diabeticandSTZ-diabeticmice/kidneycapsuleYesPagliucaetal.
[23]HUES8[hESC];hiPSC-1,hiPSC-2[hiPSCline]SuspensioncultureonastirplateINS+,GCG+,SST+>30%Yes(invitroandinvivo)SCID-beigeanddiabeticmice(NRG-Akita)/kidneycapsuleYesShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page5of19Table1Generationofinsulin-positiveβ-likecellsfromhESC/iPSC,theirmaturation,andfunctionsinvitroandinvivo(Continued)References[Celllinesused]DifferentiationconditionCelltypesinducedPercentinsulin+cellsGSISRecipients/transplantationsiteAmeliorationofhyperglycemiaRussetal.
[2]MEL1INSGFP/W[hESCline]Low-adherenceplatesINS+,GCG+,SST+~60%Yes(invitroandinvivo)STZ-diabeticNODmice/kidneycapsuleYesAgulnicetal.
[25]CyT49[hESCline]SuspensioncultureINS+,GCG+,SST+40–50%Yes(invivo)SCID-beigemice/subcutaneouswithencapsulationdevicen.
d.
Toyodaetal.
[26]KhES-3[hESCline];585A1,604B1,692D2,648B1and409B2[hiPSCline]OnMatrigel/lowadhesionplateINS+,GCG+,SST+n.
d.
Yes(invivo)NOD–SCIDmice/kidneysubcapsulen.
d.
Millmanetal.
[27]ND-1andND-2[NDhiPSCline];T1DhiPSClineOnMatrigel/SpinnerflasksonastirplateINS+,GCG+[n.
t.
.
:SST+]24–27%Yes(invitroandinvivo)ND-SCIDmiceandalloxan-induceddiabeticmice/kidneycapsuleYesManzaretal.
[28]T1DhiPSClineMatrigel/3DcultureINS+,GCG+,SST+~56%Low(invitro)ImmunodeficientSTZ-diabeticmice/shoulderregionYesYabeetal.
[29]TkDN4-M,253G1,454E2[hiPSCline]OnMatrigel/aggregateonultra-lowadhesionplateINS+,GCG+,SST+30–33.
6%Yes(invitro)STZ-diabeticNOD-SCIDmice/kidneycapsulesYesPercentagesofinsulin-positivecells,glucose-stimulatedinsulinsecretion(GSIS),andinvivofunctionsreportedfromvariousstudiesaresummarizedMEFs,mouseembryonicfibroblasts;INS+,insulin-positivecells;GCG+,glucagon-positivecells;SST+,somatostatin-positivecells;PPY+,pancreaticpolypeptide-positivecells;GHRL+,ghrelin-positivecells;n.
t.
,nottested;n.
a.
,notapplied;n.
d.
,notdeterminedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page6of19efficientlyestablishedPDX1+progenitorsbyusingretin-oicacidincombinationwithinhibitorsofBMPandhedgehogsignalingpathways,whilesimultaneouslyadd-ingeitherFGF10orFGF7.
Theβ-likecellsgeneratedinsuchmonolayerculturewerelargelypolyhormonalinsulin-expressingcells(Fig.
1a).
Polyhormonalcellslackexpressionofkeyβcelltranscriptionfactorsandexhibitlimitedglucose-stimulatedinsulinsecretion(GSIS)invitro[10,32–34].
Formationofnon-functionalpolyhor-monalcellsisconsideredthelimitationoftheseproto-cols.
Whetherthecultureplatformortheinappropriatecombinationsofgrowthfactorsintheculturemediapromotesuchcellsarenotclearlyknown.
Varyingde-greesofinvitroGSISfromhESC/iPSC-derivedinsulin-positivecellshavebeenreportedbyseveralstud-ies,includinganapproximately1.
7-foldincreaseob-servedbyChenetal.
[15],a2-foldincreasenotedbyJiangetal.
[11]andZhangetal.
[16],andapparentlynoGSISreportedbyD'Amouretal.
[10]andKunisadaetal.
[17](Fig.
1a)(Table1).
Thesedifferencesandlowlevelsofsecretedinsulincouldbeduetothegenerationofvaryingnumbersofpolyhormonalcellsinculture.
Thepolyhormonalcellsmayresembletheimmatureβcellsobservedinmid-gestationhumanfetalpancreases[70,71].
Theroleandfateofpolyhormonalcellsduringhu-manfetaldevelopmentarepoorlyunderstood;however,immunohistochemicalcharacterizationindicatesthatthesecellspossessanαcelltranscriptionfactorprofile[72].
Severalreportshavedescribedtheformationofglucagon-expressingαcellsinvivofollowingtransplant-ationofhESC-derivedpolyhormonalcells[21,33,73](Fig.
1a),anddynamicchromatinremodelingwasre-portedtooccurduringthistransitionintomaturedcelltypes[73,74].
StudiesofBruinetal.
[32]revealedsev-eralkeyfeaturesofpolyhormonalinsulin-positivecellsthatdifferfromthoseofmaturepancreaticβcells,in-cludingdefectsinglucosetransporterexpression,KATPchannelfunction,andprohormoneprocessingenzymes.
Thesedeficienciesmustbeaddressedwithfurtherproto-colmodificationstogeneratehESC/iPSC-derivedpan-creaticβcellsthatshowGSISinvitro.
AlthoughseveralofthesereportsdescribedthedetectionofGSISinvitro,noneofthereportedcellswerecapableofefficientlyre-storingeuglycemiainaninvivodiabeticanimalmodel.
Toovercomethislimitation,analternativestrategytoobtainglucose-responsiveinsulin-producingcellshasbeenestablishedinseveralstudies[12,14,18–21,26](Fig.
1b).
MostofthesestudiesusedMatrigelasthe2DplatformforESC/iPSCmonolayerculture,followedbysuspensionculturewithorw/ostirringusinglowadhe-sionplate.
Continuousstirringpromotescell-cellandcell-matrixinteractionswithintheculture.
TheresultantEPcellswerethentransplantedintorecipientmiceforfurtherdifferentiationinvivo.
ThesestudiesdemonstratedthathESC/iPSC-derivedpancreaticprogenitorcellswhentransplantedintoectopicsitesinimmunodeficientortype1diabetesmice;theyunderwentfurtherdifferentiationandmaturationintoglucose-responsiveinsulin-secretingcells,whichcouldreversediabetesinrecipientmice[18,20,21](Fig.
1b)(Table1),suggestingthatpancreaticpre-cursorsorimmatureislet-likecellsobtainedinvitrocouldmatureinvivo.
Thisalsoindicatesthatsomeinvivofac-torsarestillmissingininvitrogrowthfactorcocktails.
Therefore,growthfactorsandsignalingmoleculesin-volvedinpancreasdevelopmentneedtobebetterscreenedtodetecttheirpotentialabilitiestocausehESC/iPSCtodifferentiateintomaturepancreaticβcellsinvitro.
Inrecentyears,tremendoussuccesshasbeenachievedinestablishingdifferentiationprotocolsthatcangenerateglucose-responsiveinsulin-secretingβcellsfromhESC/iPSCinvitroexpressingmatureβcellmarkers,andameli-oratinghyperglycemiaindiabeticmicefollowingtrans-plantationofthesecells[2,22,23,29](Fig.
1c)(Table1).
Inthesestudies,hESCs/iPSCswereculturedeitherinlowad-hesionplateorinthree-dimensional(3D)suspensioncul-turewithcontrolledstirring,whichpromotecell-cellandcell-matrixinteractionsresultingintheformationofcellag-gregates.
Sequentialandtime-dependentuseofsignalingmoleculesinsuchculturesystemsconcurrentlyguideshESC/iPSC-derivedcellstoappropriatelydifferentiateto-wardspancreaticβcellswithbetterphenotypesinvitro.
Aftertransplantationintorecipientmice,cellsresidingintheaggregatesunderwentfurtherdifferentiationandmatur-ationintomatureβcells.
Thesesimplifieddifferentiationconditionsenabletheefficientgenerationofhumanpancre-aticandmorerestrictedendocrineprogenitorpopulationsfrompluripotentstemcellswithoutunwantedformationofpolyhormonalcells.
Furthermore,theinducedβcellsinthisprotocolshowbothinvitroandinvivogeneexpressionpatterns,ultrastructuralcharacteristics,andglucoserespon-sivenesstoinsulinsecretionthatcloselyresemblethoseofβcellsfrompancreaticislets[2,22,23].
Moreover,com-paredtopreviouslyreportedimplantationsofhESC/iPSC--derivedpancreaticprogenitors,forwhichittook3–4monthsafterimplantationforcellstomature,recentad-vancesinthegenerationofβcellsinvitrosubstantiallyshortenthewaitingtimetotherapeuticeffectsafterim-plantation.
Inastudy,Rezaniaetal.
[22]optimizedtheirpreviousdifferentiationprotocolbyaddingfactorssuchasvitaminC,proteinkinaseCactivators,transforminggrowthfactor-βreceptorinhibitors,andthyroidhormonestogen-erateinsulin-producingcellsataninductionrateofap-proximately50%.
Furthermore,theyidentifiedR428,aselectivesmall-moleculeinhibitoroftyrosinekinaserecep-torAXL,asacrucialfactorforthematurationofβcellsinvitro.
Pagliucaetal.
[23]alsooptimizedadifferentiationmethodtogenerateβcellsfromhESC/iPSCinvitroatanShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page7of19inductionefficiencyof>30%.
Inthisstudy,ascalablesuspension-basedculturesystemthatadoptedfromSchulzetal.
[19]wasusedtogeneratemorethan108hPSCsforfurtherdifferentiation.
Thisprotocoltakes4–5weeksandinvolvesauniquecombinationofsequentialculturestepsusingfactorsthataffectsignalinginnumerouspathways,includingsignalingbyWnt,activin,hedgehog,EGF,TGFβ,thyroidhormone,andretinoicacid,aswellasγ-secretaseinhibition.
Later,in2015,Russetal.
[2]showedthattheuseofBMPinhibitorstospecifypancreaticcellspromotestheprecociousinductionofendocrinedifferentiationinPDX1+pancreaticprogenitors,whichultimatelyresultsinthefor-mationofnon-functionalpolyhormonalcells.
Therefore,intheirculturesystem,thecommonlyusedBMPinhibitorswereomittedduringpancreaticspecification,whichpreventprecociousendocrineformation,whiletreatmentwithret-inoicacidfollowedbycombinedEGF/keratinocytegrowthfactor(KGF)efficientlygeneratesbothPDX1+andsubse-quentPDX1+/NKX6.
1+pancreaticprogenitorpopulations,respectively.
TheprecisetemporalactivationofendocrinedifferentiationinPDX1+/NKX6.
1+progenitorsfinallypro-ducesglucose-responsiveβ-likecellsinvitroataninduc-tionefficiencyof~60%.
Thus,thisprotocolisconsideredtobemorecloselyresembleskeyaspectsofearlyhumanpancreasdevelopmentand,assuch,representsanimprove-mentoverpreviousprotocols.
Alltheseobservationssug-gestthatinsulin-producingcellssuitablefordiabetescelltherapiescanbeproducedfromhESC/iPSCinvitro.
How-ever,theformationofhESC/iPSC-inducedβcellsinvitrodependsonmultiplefactors,suchastheuseofplatforms/materials,applicationofsuspensionculture,useofalargenumberofgrowthfactorsandtheircombinations,andthetimingofrotatingthecultures.
Inthesemultistageproto-cols,althoughthefinalcellpopulationhasonlyabout30–60%β-likecells,themajorityoftheremainingcellpopula-tioncomprisedrelativelyuncharacterizedcellsthatmaybeundifferentiatedprogenitorsorothertypesofunwantedcells.
Thus,improvingdifferentiationefficiencytogeneratehigherpercentagesofβcellsinvitroremainsanimportantchallenge.
AsimilariPSC-derivedβcellgenerationprotocolhasbeenreportedforpatientswithtype1diabetes(T1D)[27,28].
Millmanetal.
[27]reportedthattheinducedcellsexpressβcellmarkers,respondtoglucosebothinvitroandinvivo,preventalloxan-induceddiabetesinmice,andrespondtoseveralcategoriesofantidiabeticdrugs.
NomajordifferenceswereobservedinT1Dstemcell-derivedβcellscomparedtostemcell-inducedβcellsderivedfromnon-diabeticpatients.
Furthermore,T1DiPSC-derivedβcellsrespondedtodifferentformsofβcellstressinaninvitrodiseasemodel.
Manzaretal.
[28]generatedglucose-responsiveinsulin-producingcellsvia3Dculture.
Inthisstudy,T1DiPSCswereini-tiallyresistanttodifferentiation,buttransientdemethylationtreatmentsignificantlyenhancedtheyieldofinsulin-producingcells.
Thecellsrespondedtohigh-glucosestimulationbysecretinginsulininvitro.
Theshape,size,andnumberoftheirgranuleswereiden-ticaltothosefoundincadavericβcells.
Whentheseinsulin-producingcellsweretransplantedintoimmuno-deficientmicethathaddevelopedstreptozotocin(STZ)-induceddiabetes,hyperglycemiadecreaseddra-matically,sothatthemicebecomenormoglycemic.
Thus,T1DiPSC-derivedβcellsareasuitablecandidateforuseasanautologouscellsourceforthetreatmentofdiabetes.
However,amoreefficientculturesystemisre-quiredtogeneratefunctionalandterminallydifferenti-atedβcellsforfutureresearchandclinicalapplications.
IsletorganoidgenerationfordiabetestreatmentPancreaticisletsarecomposedofECs,includinginsulin-producingβcells,glucagon-producingαcells,somatostatin-producingδcells,pancreaticpeptide-pro-ducing(PP)cells,andghrelin-producingεcells[75–77].
Afterfunctionalmaturation,theseECsintheisletshelptoregulatebloodglucoselevels.
ReciprocalinteractionsamongECsintheisletsarecriticalforregulationofin-sulinsecretioninresponsetoglucose[78–80].
Thus,pancreaticisletstructuresofferaneffectivemeansofphysiologicallyregulatinginsulinsecretioninpatientswithdiabetesmellitus.
Organoidsareagroupofprimarycells,ESCs,oriPSCsgrowninvitrothatowetheirself-renewalcapacitiesandabilitytodifferentiateinto3Dstructuresthatassumeasimilarorganizationandfunctionalityasanorgan.
Thegenerationofisletorganoidscontainingmatureβcellswithfullfunctionalityisyettobedemonstrated.
How-ever,generatingsuchfunctionalorganoidswouldbevaluableinperformingpathologystudiesofdiabetesde-velopment,treatment,anddrugscreening[81,82].
Inthelastdecade,severalresearchgroupshavereportedonthegenerationofhESC/iPSC-derivedislet-likeclus-ters/aggregates,aswellasislet-likeorganoids[81–87].
Intheearlystudies,onlythefeasibilityofgeneratingislet-likeclustersoraggregatesfromhESC/iPSCwasstudied.
However,inrecentyears,considerablesuccesshasbeenachievedingeneratingislet-likeorganoids(Fig.
3).
Islet-likeorganoidsdevelopedfromhPSCbyKimetal.
[86]showedglucoseresponsivenessinvitro,aswellasinvivo.
Inthatstudy,ECsexpressingpancre-aticendocrinehormoneswerefirstgeneratedfromhESCandiPSCusingastep-wiseprotocol,andECclusters(ECCs)werethenformedspontaneouslyin1dayfromthedissociatedECsinanoptimized3Dculture.
ThesizesofthehESC-derivedECCswereapproximately50–150μmindiameter,whichissimilartothesizesofhu-manpancreaticislets.
TheECCscomprisedseveralpan-creaticECtypes,exceptforαcells,andthusshowedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page8of19thathESC-derivedECCsare,tosomeextent,analogoustohumanpancreaticisletsintermsofsizeandcellcom-position.
Levelsofβcell-associatedgenetranscriptionandGSISwerefoundtobehigherinECCsthaninECs.
Inaddition,intracellularCa2+influxoscillatedinECCsduringglucosestimulation,andSTZ-treateddiabeticmicetransplantedwithECCsbecamenormoglycemicwithin3daysaftertransplantationandsurvivedforap-proximately2months.
Thisstudy,therefore,supportedtheideathatfunctionalislet-likeorganoidscanbegener-atedfromhPSCs,whichcouldserveasanalternativesourceoftherapeuticcellsforthetreatmentofdiabetes.
AnotherstudybyWangetal.
[81]demonstratedthede-velopmentofisletorganoidsfromhESCin3Dbiomim-eticscaffoldsusingseveralgrowthfactors,whichpromotepancreaticECdifferentiation.
Theorganoidsformedinthisstudyconsistedofpancreaticα,β,δ,andPPcells,and,importantly,mostinsulin-secretingcellsgenerateddidnotco-expressglucagon,somatostatin,orPP.
Matureβcellmarkergeneswereexpressed,andinsulin-secretorygranules,whichareindicationsofβcellmaturity,weredetectedinthese3D-inducedcellclus-ters.
The3D-inducedorganoidcellsweresensitivetoglucoselevels;exposingthecellstoahighconcentrationofglucoseinducedasharpincreaseininsulinsecretion.
However,theseisletorganoidswerenottransplantedintoanimalmodelstoconfirmtheirbiologicalfunction.
Theconventional2Dcultureofstemcellsoverseveralpassagesinfluencecellphenotypeandfunction[88].
Cellsareonlypartiallypolarizedonaflatsubstrate.
Incontrast,3Dcellcultureonaspecializedmatrixpreventscellsfromattachingtothebottomoftheplatebymain-tainingthecellsinsuspensionorembeddingtheminthematrixinwhichcell-cellandcell-matrixinteractionsaremaintained,therebypromisesphenotypicmainten-anceandself-assemblyoffunctionaltissue-likepolarizedstructures[89–91].
3Dplatformsrecapitulatemechan-icalandbiochemicalstimuliaspresentinnativetissueandthusdictatepolarization[92].
However,suchstruc-turesoftendonotentirelymatchmulticellularorganizationseeninnativetissue.
Extracellularmatrix(ECM)isacriticalregulatorofcellularprocesseswhichservediversefunctionssuchassequesteringsignalingmoleculesandtransmittingligand-specificcuesviacellreceptorsandisamenabletosynthesis,degradation,andreassemblyovertime[93].
Cellsreadilyshapeandre-modeltheirextracellularenvironmentbyenzymaticallydegradingandresynthesizingtheECM.
Intissues,ECMnotonlyactsasanimmobilizationplatformforahigherorderofself-assemblybutalsofacilitatestherelayofabFig.
3Schematicoffabricationprocessesforislet-likeorganoids,adoptedandmodifiedfromCandielloetal.
[82]andTakahashietal.
[87].
aGenerationofhESC-derivedisletspheroidsandislet-likeorganoidsonAmikagelhydrogelplatform.
Pre-differentiatedhESC-derivedpancreaticprogenitorcells(hESC-PPs)on2DMatrigelwereharvestedandthenseededontotheAmikagelhydrogelplatformtoeitherformhomogenousisletspheroidsorbecombinedwithendothelialcells(HUVEC)toformendothelializedheterogeneousislet-likeorganoids.
Severalotherscaffold-basedstrategieshavealsobeenappliedtogeneratehESC-derivedislet-likeorganoidssuchascollagen-Matrigelscaffolds.
bGenerationofvascularizedislet-likeorganoidsinself-condensationculture.
Inthisprocess,isolatedadultmouse/humanisletsorhiPSC-derivedpancreatictissueswereco-culturedwithendothelialcells(HUVECs)andhumanmesenchymalstemcells(hMSCs).
Inthebeginning,thecellswerescatteredthroughouttheculturewell,andthen,theybeganmovingtowardsthecenterofthewelltoformcondensedtissue.
EachcondensedtissuecontainedpancreaticisletswithendothelialcellssurroundingthemShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page9of19biochemicalandmechanicalcuesinabufferedandhy-dratedenvironment[93].
ECMinteractionshavebeenshowntoimproveβcellproliferation[94],insulinsecre-tion[95,96],andisletdevelopment[96–98].
Collagenhasbeenusedwidelyfor3Dstemcellcultures[99].
Acollagenscaffoldconstitutesasoftandflexiblefibrousnetworkthatmaintainscellmorphologyandallowscellstofreelyreachout,migrate,andform3Dstructures.
However,collagenaloneisinsufficienttoprovidemul-tiplecuesandsophisticatedgeometryandcompositionthatexistinanativeextracellularmatrix.
Inpreviousstudies,thecombinationofcollagenwithMatrigel,acomplexheterogeneousmixtureofbasementmembraneproteinssuchaslaminin,collagenIV,fibronectin,hep-arinsulfateproteoglycans,andentactin,hasbeenusedastheunderlyingmaterialtoreconstructcardiacmuscleanduterinetissuesinvitro[100,101].
Inastudy,Wangetal.
[81]usedafour-stagedifferentiationstrategytodifferentiatehESCintopancreaticendodermandtoma-turethesecellsintoisletorganoidswithincollagen-Matrigelscaffolds.
Theirresultsshowedthataugmenta-tionofcollagenscaffoldswithMatrigelcreatesbetter3DnichesforisletorganoiddevelopmentfromhESC.
Al-thoughneitherMatrigelnorrattailcollagenIisaUSFoodandDrugAdministration-approvedmaterialforclinicalapplications,thestudyonlydemonstratedthefeasibilityofgeneratingisletorganoidsfromhESC.
How-ever,thecellclusterscanbepurifiedbyenzymaticallydigestingthescaffolds.
AnotheralternativeistouseaporcinedecellularizedECMtoconstructscaffolds.
Ashortageofdonorisletsiscurrentlylimitingthewide-spreadimplementationofislettransplantationtotreatdia-betes[102].
Inresponsetotheseneeds,recentstudieshavefocusedprimarilyonderivingisletβcellsfromhESC/iPSCasanalternativetodonorislets[2,22,23,27–29].
Thenon-endocrinecomponentsofisletsalsoplayacriticalroleintheirfunction.
Previously,heterogeneouspancreaticorganoidshavebeengeneratedbyaggregatingadultmouseβcellswithendothelialandmesenchymalcells[103].
Theseorganoidswerefoundtosuccessfullyintegratewithhostvasculatureandnormalizebloodglucoseindiabeticmice.
Systematicgenerationofheterogeneousorganoidsinvitrorequiresanorgan-specificcellsourceanda3Dcultureplat-formtoinduceself-organization,lineagespecification,func-tionalmaturationoforgan-specificcells,andintegrationofsupportingcellpopulations[104,105].
Scaffold-basedstrat-egieshaveprimarilyreliedonlaminin-richMatrigel,aswellasothernaturalorsyntheticbiomaterials,whichtypicallyconfinedcellswithinthe3Dscaffold.
Recently,isletorga-noidshavebeengeneratedfromhPSCsbyaggregatingthesecellsintohomogenous3Dislet-likespheroidsusing2Dnon-adherentculture[86]orbyembeddingtheminacollagen-Matrigelmatrix[81].
Effectivebioengineeredplat-formsthatwillsupportspecificorganoidproduction,finecontrolovertheorganoidsizeandcellularcomposition,scalingupofproduction,andeaseoforganoidrecoveryafterculturearestillneeded.
Hydrogelshavebeenafavoredchoiceofmaterialsintissueengineeringapplicationsduetotheirabilitytomimicthearchitectureandmechanicsofpli-ablecellularmicroenvironment[106,107].
Tissue-likeflu-idity,faciletransportofsolublenutrients,easeoffabrication,andintegrationwithbiologicalinterfacesaresomeofthemainadvantagesofahydrogelsystem.
Inare-centstudy,isletorganoidsofaprecisesizeandcellularhet-erogeneitywereengineeredfromhESC-derivedpancreaticisletcellsutilizinganovelhydrogelplatform,Amikagel[82](Fig.
3).
TheAmikagel-basedplatformwasshowntofacili-tatecontrolledandspontaneous,ratherthanforced,aggre-gationofhESC-derivedpancreaticprogenitorcells(hESC-PPs)intorobusthomogeneousspheroids.
Thefor-mationofAmikagel-inducedhESC-PPspheroidsenhancedpancreaticislet-specificPDX1andNKX6.
1geneandpro-teinexpression,whilealsoincreasingthepercentageofcellsco-expressingboth.
Amikagelalsoenabledco-aggregationofhESC-PPwithsupportingendothelialcells,resultinginself-organizedmulticellularpancreaticorganoidsthatwereclosertoisletphysiologyintermsoftheirheterogeneitythanhPSC-PPhomogenousspheroids.
.
TheseAmikagel-in-ducedhESC-PPspheroidsandheterogeneousorganoidsspontaneouslydifferentiatedintomatureβ-likecellsthatshowexpressionoftheβcell-specificINS1gene,aswellasC-peptideprotein,andproduceinsulininresponsetoinvitroglucosechallenge.
Aftermaturation,theAmikagel-in-ducedheterogeneousorganoidsalsoshowasignificantlydevelopedextracellularmatrixsupportsystem.
Therefore,theAmikagelplatformcouldbeidealforengineeringmulti-cellular3DisletorganoidsfromhPSCs.
Thepurposeforin-ducingandmaintaining3D-aggregatedorganoidsistoenhancetissue-ororgan-specificfunctionsbyreproducingcells'nativeenvironments.
Commonlyusedtechniquesforengineeringisletspheroidsneitherhaveprecisecontrolovertheultimatesizeofanaggregate,nordotheysupportcellinclusion,whichisthenextstepneededtogenerateisletorganoidswithmulticellularcomplexityandeventualgenerationofvascularizedconstructs.
TheAmikagelplat-formisparticularlysuitableinthiscontext.
Adevelopedextracellularmatrixbaseisimportantforisletstructure,cellhealth,andoverallfunction,whilealsobeingaprerequisiteforadevelopedvascularsystem[108].
Integrationofendothelialcellswouldbeanim-portantinitialsteptowardsvasculardevelopment[109].
Inthecontextofregenerativemedicine,tissuesurvivalandneovesselorganizationofhESC-derivedcellsmaybedependentonendothelialinclusionandmesenchymalsupplementation[110].
In2018,acomplexorganoiden-gineeringmethodtogeneratepancreaticisletswasre-ported[87](Fig.
3).
Usingthisprotocol,pancreaticislet-likeorganoidswithvascularnetworkswereformedShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page10of19byco-culturingeitherisolatedadultmouse/humanislettissuesorhiPSC-derivedpancreatictissueswithvascularendothelialcells(HUVECs)andhumanmesenchymalstemcells(hMSCs).
Pancreaticislet-likeorganoidsweregeneratedbyself-condensationafterseedingcellsontotheMatrigelbed.
Transplantationofthesevascularizedislet-likeorganoidsintothekidneysubcapsuleoffulmin-anttype1diabeticmicesignificantlyimprovedthesur-vivalofthediabeticmiceandeffectivelynormalizedbloodglucosecomparedtoconventionalislettransplant-ation.
Thisapproach,therefore,offersapromisingalter-nativetotherapeuticislettransplantation.
Thefunctionalityofisletorganoidsgeneratedsofarremainspartial.
Someofthelimitationsoftheseorganoidsarethattheyoftenlackcelltypesneededforcompleteisletfunctionsandthegenerationofbloodvesselsandnerves.
Toapplyisletorganoidstothetreatmentofdia-betes,morecompleteisletstructuresmustbepreparedforbetterfunctionindiabeticrecipients.
Despitethepromiseofemergingisletorganoid-basedapproaches,developingvascularnetworksremainsamajorchallengetotheirapplicationinregenerativetherapies.
ESC/iPSC-derivedβcellsfordiabetestreatment:limitationsandchallengesTherearestillmanypointstoaddressandproblemstoovercomebeforehESC/iPSC-derivedcellscanbeclinic-allyappliedindiabeticpatients,includingthefollowing:(1)Safetyissues:Sofar,mostpatient-specificiPSCshavebeenestablishedwithretrovirusvectors.
TheseiPSCshavenumeroustransgeneintegrationsintheirgenomes,andtheseintegrationsmaycauseleakyexpressionthatcaninterruptthefunctionofendogenoustranscriptionfactornetworksandleadtodifferentiationfailure.
An-otherimportantproblemoftransgeneintegrationistumorigenicriskaftertransplantation.
Inparticular,c-Myc,oneofthereprogrammingfactors,isawell-knownoncogene,anditsreactivationcangiverisetotransgene-derivedtumorsinchimericmice[111].
TomakesafeiPSCs,oneimportantapproachmaybeelim-inatingthec-Myctransgeneinthereprogrammingcock-tail.
HumanandmouseiPSCscanbeestablishedfromfibroblastswithonlyOct3/4,Sox2,andKlf4,butboththeefficiencyofiPSCgenerationandthequalityofthesecellsaresignificantlyreduced[112].
Chimericmicepro-ducedwithc-Myc-freeiPSCsdidnotshowenhancedtumorformationincomparisonwithcontrolmice.
How-ever,retroviralinsertionsinthegenomeitselfmaydis-turbendogenousgenestructureandincreasetheriskoftumors[113].
ToincreasethesafetyofhiPSC-basedcelltherapies,itisnecessarytogeneratehiPSCswithoutvec-torintegrationandcontinuousc-MYCexpression.
ThegenerationofhiPSCswithtransientexpressionfromnon-integratingvectors[52,56,114]mayaddresstheseconcerns.
Todate,variousintegration-freetechniqueshavebeenreported,includingtransientexpressionofre-programmingfactorsusingadenovirus[115]orSendaivirusvectors[116],thepiggyBacsystem[51],episomalvectors[52,56],aminicirclevector[53],anddirectde-liveryofprotein[50]orsyntheticRNA[54].
However,theiriPSCinductionefficienciesarelowerthanthosewithretrovirusvectors,possiblybecauseoflowtrans-ductionefficiencyandunstableexpression[117].
(2)Variationindifferentiationefficiencies:DifferentiationpropensitiesarereportedtovaryamonghESClines[118].
Dependingonthecelloriginorderivationproced-ure,someiPSClinesalsodemonstratevaryingdegreesofdifferentiationefficiency,resistancetodifferentiation,ortumorigenicity[65,84].
Abnormalitiesinkaryotypeandvariationsinthetechniquesusedtoobtainormain-tainiPSClinesandepigeneticdifferencesamongthemhavealsobeenconsideredvitalfactorsthatalterdiffer-entiationpotential.
Epigeneticvariationsaremorepro-nouncediniPSCthanESC.
Thus,selectionofgoodiPSClineswithlowbatch-to-batchvariationindifferen-tiationefficiencyisessentialtodifferentiatingthesecellsintotargetlineagespriortouseinspecificcelltherapies[118].
Inaddition,differentiatedcellspreparedfrompatient-specificiPSCcanincreasethesuccessrateofcelltherapiesinthefuture.
(3)Formationofpolyhormonalcells:Polyhormonalinsulin-expressingcellsarefre-quentlyformedfromhESC/iPSC-derivedcellsinvitro,asdiscussedabove.
AvailablereportssuggestthatoncehESC/iPSC-derivedcellsbecomepolyhormonal,theycannotbedifferentiatedintomatureβcells[33].
There-fore,itisnecessarytofindouttherightcombinationoffactorstoreducetheformationofpolyhormonalcellsinculture,aswellastoinducethesecellsintomatureβcellsiftheyaregenerated.
(4)Xenogeneiccontamina-tionsandunknowneffects:Althoughmostrecentdiffer-entiationprotocolshavebeendevelopedonfeeder-freeculturesystems,manyprotocolsstillcallforavarietyofundefinedanimal-derivedproductsthatmayhaveun-knowneffectsoncellcharacteristicsanddifferentiationability.
Thepotentialconsequencesoftransplantinghu-mancellsexposedtoanimal-derivedproductsintopa-tientscouldincludeincreasedriskofgraftrejection,immunoreactions,microbialinfectious,prions,andyetunidentifiedzoonoses[119–121].
Toreducetheeffectsofxenogeneiccontamination,Micallefetal.
[122]usedxeno-freemedia;however,theyusedMEFforpassaging.
Inanotherstudy,Schulzetal.
[19]expandedhESCinxeno-freemediawithoutfeedercells,buttheyusedfetalbovineserumduringdifferentiation.
Later,Shahjalaletal.
[24]expandedanddifferentiatedhESCandiPSCinasyntheticscaffoldundercompletelyxeno-freeconditionsusingrecombinantand/orhumanizedcomponentsandsuccessfullygeneratedinsulin-expressingcellsinvitro.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page11of19ThesestudiesindicatethefeasibilityofgeneratinghESC/iPSC-derivedpancreaticβcellsunderxeno-freecondi-tions.
Forsuccessfulclinicalapplications,hESC/iPSCshouldbeprepared,maintained,anddifferentiatedinxeno-freeculturesystems.
Humanizedand/orrecombin-antfactors,chemicallydefinedsupplements,andsyn-theticscaffoldscanbeappliedinvitrotoaddressthisissue.
(5)Lackofmaturation:Todate,insulin-expressingcellsgeneratedfromhESC/iPSCinvitrolacktheproper-tiesofmaturepancreaticβcells.
Transplantationofim-maturehumanislet-likecellstoimmunodeficientmiceenablesfurthermaturationofisletcells.
Thisisevi-dencedbyhumanC-peptidesecretioninglucosetoler-ancetestsandbymorphologicalandultrastructuralstudies[2,22,23,123].
Itisimportanttounderstandwhatfactorsintheinvivomilieuarecriticaltofunc-tionalmaturation.
Thesecouldberelatedtolocalsignalsprovidedbytheinvivonicheatthetransplantsite.
Re-cently,ithasbeenshownthatmaturationoccursfasterandmoreefficientlyinfemalerecipientmice,pointingtothepotentialroleofestrogenreceptorsignalinginmaturation[124].
Geneprofilingstudiessuggestthatthecreationofmatureβcells,inwhichinsulinsecretionistightlycoupledtoglucoseconcentrations,requiresthecoordinatedupregulationofcertaingenesandrepressionofothers[125].
Arecentreportshowedthatligand-dependenttranscriptionfactorestrogen-relatedreceptor-γ(ERRγ)isadriveroftheoxidativemetabolicgenenetworkinmatureβcellsandthatitspostnatalin-ductionorchestratesthemetabolicmaturationofβcells[123].
Thisreportalsoindicatedthatβcell-specificERRγ-deficientmiceareglucoseintolerantandfailtoappropriatelysecreteinsulininresponsetoglucosechal-lenge.
ERRγexpressionduringpostnatalβcellmatur-ationdrivesatranscriptionalprogramthatpromotesthemitochondrialoxidativemetabolismnecessaryforGSIS.
Assuch,promotingERRγexpressionandactivityduringthelatestageofhiPSCdifferentiationinvitroresultsinglucose-responsiveβcellsthatarecapableofrestoringbloodglucoseintype1diabeticmice.
Thus,futurestud-iestoimprovefunctionalmaturationofinsulin-expressingcellsshouldfocusonsignalingpath-waysthatregulatethematurationofpancreaticβcells.
(6)Lowsurvivalrateandimmunogenicity:Becauseofthelackofasuitabletransplantationtechnique,there-coveryofwell-demarcatedgraftsaftertransplantationintoectopicsitesinexperimentalanimalsandexamin-ationofglucoseresponsivenessofhESC/iPSC-derivedpancreaticcellsinvivoarestilldifficult.
Thiscouldbeduetoimmunerejectioninthehostanimals.
Atpresent,twodifferenttransplantationstrategiesareapplied:oneisdirectimplantationofhESC/iPSC-derivedpancreaticcellsintoectopicsites,andotheroneisimplantationofadevicecontaininginducedpancreaticcells(Fig.
4).
Inthefirstmethod,pretreatmenttoinduceangiogenesisatimplantationsitesisusedtopromoteengraftmentandlong-termsurvivaloftheimplantedcells.
Onerecentstudyshowedthatanyloncatheterembeddedintothesubcutaneoustissuesofhostmicefor1monthbeforecellimplantationgeneratedavascularizedspace[126].
Theformationofvascularnetworksattheimplantationsiteandtheimplantationofpancreaticcellsafterinflam-matoryreactionshavediminisheddevelopealessin-tolerantenvironmentfortheimplantedcells.
Inthesecondmethod,pancreaticcellsareencapsulatedinadevicemadeofbiocompatiblematerialthatincludessemipermeablemembranes.
Oxygenandnutrientscanpassthroughthemembranestopromotecellsurvival,differentiation,andmaturation,whereasimmunemole-culesandcellscannot.
Severalstudieshaveshownthat,whenimplantedsubcutaneouslyintohostmice,hESC/iPSC-derivedpancreaticcellsencapsulatedbythesesemipermeablemembranedevicescanfurtherdifferenti-ateintomatureinsulin-secretingcellsandsurvivefromhostimmuneresponses,primarilybyTcells[20,21,25,35].
Inaddition,becauseofvasculogenesisaroundthesedevices,thedifferentiatedβcellscansecreteinsulininresponsetochangesinglucoseconcentrations.
ArecentstudyalsodemonstratedimplantationofhESC-derivedβ-likecellsencapsulatedwithanalginatederivative.
Thisdevicemitigatesforeignbodyresponsesandimplantsfi-brosis,andinducesglycemiccorrectionwithoutim-munosuppressioninimmune-competentmice[127].
Thesedevice-basedimplantationmethodscanreduceoreliminatetheneedforimmunosuppressiveagents.
Fur-thermore,thesemethodsmayhavetheadvantageofallowingremovaloftheimplantedcellswiththedevicewhenadverseeventssuchastumorigenesisordysfunc-tionoccur.
However,itispresentlyunclearwhetherpro-tectionfromsolubleantibodiesdirectedagainstdifferentiatedβcellswillbeasignificantproblem[128].
Althoughinsulin-expressingcellmaturationcanoccurwithorwithouttheimplantedcell/devicecombination,thesurvivalrateoftheimplantedcellsinhostsisstillrelativelylow.
Thus,asuitabletransplantationtechnique,alongwithaneffectivecombinationofinducers,isre-quiredtoovercomethistransplantationchallenge.
Des-piteseverallimitations,phase1/2clinicaltrialshavealreadystartedforthetreatmentoftype1diabetespa-tientsusingasemipermeablemembranecapsuledevicethatcarrieshESC-derivedpancreaticprogenitorsco-expressingPDX1andNKX6.
1[36].
Thistrialhasattractedattentionworldwide,asitrepresentsanim-portantfirststepforthedevelopmentofnewstemcelltherapiesfordiabetes.
Todate,noclinicaltrialswithhiPSC-derivedpancreaticcellshavebeencarriedout.
However,thepotentialadvantagesofhiPSCoverhESCmaymakesuchtherapiesavailableinthefuture.
(7)IsletShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page12of19βcellheterogeneity:βcellsinhumanpancreaticisletshavebeenthoughttobeahomogenouscellpopulation.
Despitethisprevailingparadigm,therehavealsobeenreportsofβcellheterogeneityinhumanislets[129,130].
Recently,astudybyDorrelletal.
hasidentifiedfourantigenicallydistinctsubtypesofhumanβcells,whicharedistinguishedbydifferentialexpressionofST8SIA1andCD9[131].
Theseβcellsubpopulationsarealwayspresentinnormaladultisletsandhavedi-versegeneexpressionprofilesanddistinctbasalandglucose-stimulatedinsulinsecretion.
Dissimilarbasalandglucose-stimulatedinsulinsecretioncharacteristicsindicatethattheβcellsubtypesarefunctionallydistinct.
Dorrelletal.
intheirstudyisolatedlivepancreaticβcellsfromhumanisletsamplesbyFACSandco-labeledthemwithantibodiesrecognizingST8SIA1andCD9andfi-nallyidentifiedfourantigenicallydistinctβcellsubpopu-lations.
TheyalsoaccessedtheexpressionofST8SIA1andCD9insectionsofhumanpancreasandfurtherconfirmedtheexistenceoffourdistinctβcellsubpopulationsinhumanislets.
TranscriptomeanalysesbyRNAsequencingoftheβcellsubsetshaveshownthatmostofthedifferentiallyexpressedgenesareofun-knownfunctioninβcells,butsomehavebeenclearlyassociatedwithinsulinsecretionorareknowntobedys-regulatedintype2diabetesmellitus.
Dorrelletal.
havealsoobservedthatthefrequenciesofβcellsubtypesarealteredinthemajorityofindividualswithtype2dia-betes.
Thus,theβcellsubpopulationsmayhaverele-vancetodiabetesandthisissueneedstobeaddressedbyextensiveresearch.
AlmostallpreviousstudieshaveattemptedtogeneratematureβcellsfromhumanESCs/iPSCs.
Recently,researchersaremainlyfocusingoneffi-cienttechniquestoenhancetheyieldofmatureβcellsandtheirsuccessfulsurvivalpost-transplantationtore-tainnormoglycemiaindiabetes.
However,βcellhetero-geneityisanemergingissue.
Thedistinctpropertiesofhumanβcellsubtypesfoundinhumanisletslikelyhaveanimportantimpactonmetabolicregulationandhu-mandiseaseprocesses.
Thus,futurestudiesshouldfocusabFig.
4MethodsforimplantinghESC/iPSC-derivedpancreaticcells.
Twodifferentmethodshavebeenapplied.
Inonemethod,hESC/iPSC-derivedpancreaticcellsareimplanteddirectlyintotransplantationsitesorintopre-developedvascularizedsitesofdiabeticand/ornon-diabeticSCIDmice(a).
Inanothermethod,hESC/iPSC-derivedpancreaticcellsencapsulatedinimmunoprotectivesemipermeabledevicesareimplantedintoectopicsitesofSCID-Beigeand/ordiabeticmice(b).
Oxygen,nutrients,insulin,andglucosecanpassthroughthemembranesofthedevicestopromotethesurvival,differentiation,maturation,andglucose-responsiveinsulinsecretionoftheencapsulatedpancreaticcellsfollowingimplantationintothehostmice.
Inaddition,vasculogenesisoccursaroundthedevices,supportingsecretionofinsulinfromthedifferentiatedβcellsinresponsetochangesinglucoseconcentrations.
Incontrast,immunecellsormoleculessuchasantibodiesandcomplementscannotpassthroughthemembranes,preventingimmunerejectionorautoimmuneresponsesagainstthecellsShahjalaletal.
StemCellResearch&Therapy(2018)9:355Page13of19Table2StandardcriteriafordesigningandperformingfuturepreclinicalstudiesinvitroandinvivoPreclinicaltoolProsCons(challenges)Possibleimprovements-NODmouseisidealforstudyingtype1diabetesandthecharacterizationoftheimmunopathologyofthedisease.
-BioBreedingratisasuitablemodelforunderstandingthegeneticsoftype1diabetes[132]andstudyingofneuropathy-associateddiabetes[133].
-Diabetesinductioninthemurinemodelispossibleviatheexposuretocertainchemicals,namelystreptozotocinandalloxan,andthusoffersausefultoolfortestingthepotentialsoftherapeuticagentsortransplantedcellstoreduceglucoselevel.
-SomediseasesusceptibilitylociinNODmousehavenomarkedimpactinhumandisease.
-VariousdrugsandantibodytherapyshowedanexcellenteffectinNODmicebutnoeffectintheclinicaltrials[134].
-InductionofdiabetesinNODmiceiscorrelatedwithmicrobialinfections.
-Inductionofdiabetesusingchemicalsintheanimalmodelcouldshowtoxiceffectstotheotherorgans,suchasthekidney,liver,brain,intestine,andreproductiveorgans.
-Applyinghumanizedmousemodelhavingthecomponentsofthehumanimmunesystem.
-Takingintoaccountthegender-dependentdiabetespathogenicityinanimalmodels.
-Settingupnewanimalmodelsthatrecapitulatediabetespathogenesisinhuman.
-MaintainingNODmiceunderspecificpathogen-freeenvironmentduringdiabetesexperimentation.
-Consideringtoxicactionsinanimalmodelsduringthechemicalinductionofdiabetesinvivo.
PreviousreportsshowedtheoccurrenceoflymphopeniaandhighproductionofTregulatorycells[135].
-Forstudyingtype2diabetes,theoccurrenceandthecauseofobesityshouldbeconsidered.
-Studyingdiabetescomplications(neuropathy)needtoavoidselectingneuropathy-resistantmousesuchasC57BL/6strain[136].
Stemcellquality-PSCscouldobviatethehurdlesofisletapplicationsuchaslackofdonorsandweaksecretionofinsulinpost-implantation.
-ApplicationofPSCsallowstheunderstandingofpatient-specificdiseasepathogenicityandalsothedevelopmentofpotentialtherapeutics.
-GenerationofiPSCsusingintegrativeorviral-basedmethodshinderstheirclinicalapplicationindiabetestherapy.
-PSCculturesusingundefinedorxenogeneicconditionsproducecellshavingunusualcharacteristicsandpoorphenotypes,andthuscannotbeappliedintheclinic.
-Usingnon-integrativeandsafemethodsforthegenerationofiPSCs.
-DevelopingaccurateassaysforevaluatingthequalityofiPSCs,suchaskaryotyping,analysisofthepluripotencymarkers,andthedifferentiationcapacity.
-Developingefficientmethodsforheterogeneityandteratomaassays.
-Microbiologicalassaysforthedetectionofcellcontamination,suchasmycoplasmatest.
-Usingdefinedandxeno-freecultureconditions.
Organoid/spheroidculture-Organoid/spheroidcultureallowsadetailedunderstandingofdiabetespathogenicity,molecularmechanisms,anddiseasemodelandprovidesausefultoolfordrugscreening.
-Fororganoidculture,Matrigel,collagen-Matrigel,orhydrogelsaremainlyusedasaplatform.
-Applicationofanimal-derivedECMsuchasMatrigelhampersthefurtherapplicationofgeneratedorganoidsintheclinic.
-Organoidcultureiscostlyandlaboriousforthelarge-scaleproduction.
-Designingsuitablesafexenogeneicfreescaffolds(physicalcues)withgrowthfactors(biochemicalcues)forthegenerationofstemcellniche.
-Discoveringacost-effectiveagentsandprotocolsforefficientorganoidcultureatthelargescale.
-Developingefficientassaysfortheevaluationofthegeneratedorganoids/spheroidspriortotheirapplicationfordiseasemodelingordrugscreening.
DifferentiationmethodsVariousdifferentiationprotocolsaredevelopedforthegenerationofinsulin-producingβ-likecellsfromPSCsineithermonolayeror3Dcultureusingacocktailofvariouschemicals,growthfactors,inhibitors,andcytokinesinordertoemulatetheinvivosystem.
-Differentiationprotocolsdependonagentsofhighcosts.
-Manyofthedevelopedprotocolsarenotreproducible.
-Themolecularmechanismsofmostofthechemicalsusedineachstepofthedifferentiationmethodremainunrevealed.
-CharacterizingthereproducibilityofthecurrentβcelldifferentiationprotocolsfromPSCs.
-Settinguphighlyefficientprotocolsforthegenerationofmatureβcellsandtheirtransplantation.
-Cultureconditionssuchasculturemedia,celldensity,ECM,cell-cell,andcell-ECMinteractionshaveanimpactonPSCdifferentiation[68,137–139]andthusshouldbeoptimized.
-Characterizingthemolecularmechanismsofthefactorsusedinthecurrentdifferentiationprotocols.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page14of19Table2Standardcriteriafordesigningandperformingfuturepreclinicalstudiesinvitroandinvivo(Continued)PreclinicaltoolProsCons(challenges)PossibleimprovementsTransplantationdevices-Encapsulationdevicesusedforcelltransplantation,suchassemipermeablecapsuleormembrane,possessvariousfunctions[140]:Avoidingtheundesirablehostimmunereactionsagainstthetransplantedcells.
Protectingthepatientfromtumorigenicactionofstemcells.
Avoidingthelossofviabilityofthetransplantedcells.
Maintainingstableinsulinsecretion-Theencapsulationdevicesneedtheapplicationofimmunemodulatingagents.
-Encapsulationdevicesmayprovokethepatient'simmunesystemandultimatelyleadtocelldeath.
-Applyingsuitableagentswithimmunemodulatingfunctions,summarizedpreviously[140],whichprotectthetransplantedstemcellsfromrejection.
-Designinganefficientencapsulationdevicewiththefollowingfeatures:Allowingenoughbloodsupplytotheencapsulatedcells.
Havingbiocompatibility.
Avoidingthestimulationofhostimmunereactions.
Permittingtheefficienttransferofthesecretedinsulintothecirculation.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page15of19notonlyonthegenerationofmatureβcellsbutalsoontheformationofsubpopulationsofβcellsfromhumanESCs/iPSCsandrevealtheirfunctionalpropertiestopo-tentiallyapplyindiabetes.
ConclusionsTheabilitytoobtainalargenumberofmatureinsulin-producingcellsfromhESC/iPSCcouldprovideun-limitedsuppliesofsurrogateβcellstoreplacedamagedcellsinpatientswithdiabetes.
Insulin-expressingpancreaticcellsgeneratedfromhESC/iPSCtodateappearsimilartoneonatalcells.
Generatingmatureinsulin-expressingcellswiththesameGSIScapabilityasendogenousβcellsandtheirsurvivalfollowingtransplantationintoectopicsitesinexperimentalhostanimalsarechallengesforfuturere-search.
Theprocessesofβcelldifferentiationandisletorga-noidformationarecontrolledbyacomplexnetworkthatdependsontranscriptionalregulationofgenesinvolvedinpancreasdevelopment,acertaintypeandnumberofdiffer-entiationfactors,andspecifictypesandconditionsofstemcellculture.
Althoughmanyfactorsareimportantforthesuccessfulgenerationandtransplantationofinsulin-secret-ingβcellsorislet-likeorganoids,asuitablecombinationoffactorsandconditionsstandsoutasoneofthemostcriticalfactors.
Thus,moreworkisneededtoincreasematurityandpost-transplantsurvivalofhESC/iPSC-derivedinsulin-producingcellsorislet-likeorganoidsthoseresem-bleendogenouspancreaticβcellsorislets,respectively.
Toachievethisgoal,chemicalscreeningofvariousregulatoryfactorsandsmallmoleculesinlatestagesofdifferentiationinvitromaybeagoodoption.
AlistofstandardcriteriafordesigningandperformingfuturepreclinicalstudiesforhPSC-derivedβcells/isletorganoidsinvitroandinvivoisgiveninTable2.
Althoughanumberofconsiderationscur-rentlylimittheuseofhESC/iPSC-derivedcellsincellre-placementtherapies,priorityshouldbegiventotheissuesdiscussedabove.
AbbreviationsBMP:Bonemorphogeneticprotein;DE:Definitiveendoderm;EC:Hormone-expressingendocrinecells;ECCs:Endocrinecellclusters;ECM:Extracellularmatrix;EGF:Epidermalgrowthfactor;EP:Endocrineprogenitor;ERRγ:Estrogen-relatedreceptor-γ;ESC:Embryonicstemcells;FGF:Fibroblastgrowthfactors;GCG+:Glucagon-positivecells;GHRL+:Ghrelin-positivecells;GLP-1:Glucagon-likepeptide-1;GSIS:Glucose-stimulatedinsulinsecretion;HGF:Hepatocytegrowthfactor;HUVEC:Humanumbilicalveinendothelialcell;INS+:Insulin-positivecells;iPSC:Inducedpluripotentstemcells;KGF:Keratinocytegrowthfactor;MEFs:Mouseembryonicfibroblasts;MSCs:Humanmesenchymalstemcells;ND:Non-diabetic;NKX6.
1:NK6homeobox1;NOD:Non-obesediabetes;PDX1:Pancreas/duodenumhomeobox1;PG:Primitiveguttube;PI3K:Phosphatidylinositol-3-kinase;PP:Pancreaticprogenitor;PPY+:Pancreaticpolypeptide-positivecells;PSC:Pluripotentstemcell;SCID:Severecombinedimmunodeficiency;SST+:Somatostatin-positivecells;STZ:Streptozotocin;T1D:Type1diabetes;TGF-β:Transforminggrowthfactor-β;Wnt:WntsignalingAcknowledgementsTheauthorsthankGarrySweeneyforcarefulproofreadingofthetext.
FundingThisworkwassupportedbygrantsfromtheNationalResearchFoundation(NRF)fundedbytheKoreangovernment(2017M3A9C6029562and2015R1A5A1009701).
AvailabilityofdataandmaterialsDatasharingisnotapplicabletothisarticleasnodatasetsweregeneratedoranalyzedduringthecurrentstudy.
Authors'contributionsHMScontributedtotheconception,draft,andmodificationofthemanuscript.
AADcontributedtothedraftandmodificationofthemanuscript.
KMNandTJcontributedtothecollectionandsortingofthedata.
SGCcontributedtothetop-layerdesignandcriticalreviewofthemanuscript.
Allauthorsreadandapprovedthefinalmanuscript.
EthicsapprovalandconsenttoparticipateNotapplicable.
ConsentforpublicationNotapplicable.
CompetinginterestsTheauthorsdeclarethattherearenocompetinginterests.
Publisher'sNoteSpringerNatureremainsneutralwithregardtojurisdictionalclaimsinpublishedmapsandinstitutionalaffiliations.
Authordetails1DepartmentofStemCell&RegenerativeBiotechnologyandIDASI(IncurableDiseaseAnimalmodel&StemcellInstitute),KonkukUniversity,120Neungdong-ro,Gwangjin-gu,Seoul05029,SouthKorea.
2DepartmentofBiochemistryandMolecularBiology,JahangirnagarUniversity,Savar,Dhaka1342,Bangladesh.
References1.
DonathMY,HalbanPA.
Decreasedbeta-cellmassindiabetes:significance,mechanismsandtherapeuticimplications.
Diabetologia.
2004;47:581–9.
2.
RussHA,ParentAV,RinglerJJ,etal.
Controlledinductionofhumanpancreaticprogenitorsproducesfunctionalbeta-likecellsinvitro.
EMBOJ.
2015;34:1759–72.
3.
PosseltAM,SzotGL,FrassettoLA,etal.
Islettransplantationintype1diabeticpatientsusingcalcineurininhibitor-freeimmunosuppressiveprotocolsbasedonT-celladhesionorcostimulationblockade.
Transplantation.
2010;90:1595–601.
4.
BartonFB,RickelsMR,AlejandroR,etal.
Improvementinoutcomesofclinicalislettransplantation:1999–2010.
DiabetesCare.
2012;35:1436–45.
5.
ShapiroAM,RicordiD,HeringBJ,etal.
InternationaltrialoftheEdmontonprotocolforislettransplantation.
NEnglJMed.
2006;355:1318–30.
6.
ShapiroAM.
Stateoftheartofclinicalislettransplantationandnovelprotocolsofimmunosuppression.
CurrDiabRep.
2011;11:345–54.
7.
WhiteSA,ShawJA,SutherlandDE.
Pancreastransplantation.
Lancet.
2009;373:1808–17.
8.
McCALLMD,TosoC,BaetgeEE,etal.
ArestemcellsacurefordiabetesClinSci.
2010;118:87–97.
9.
Dominguez-BendalaJ,InverardiL,RicordiC,etal.
Stemcell-derivedisletcellsfortransplantation.
CurrOpinOrganTransplant.
2011;16:76–82.
10.
D'AmourKA,BangAG,EliazerS,etal.
Productionofpancreatichormone-expressingendocrinecellsfromhumanembryonicstemcells.
NatBiotechnol.
2006;24:1392–401.
11.
JiangW,ShiY,ZhaoD,etal.
Invitroderivationoffunctionalinsulin-producingcellsfromhumanembryonicstemcells.
CellRes.
2007;17:333–44.
12.
ShimJH,KimSE,WooDH,etal.
Directeddifferentiationofhumanembryonicstemcellstowardsapancreaticcellfate.
Diabetologia.
2007;50:1228–38.
13.
EshpeterA,JiangJ,AuM,etal.
Invivocharacterizationoftransplantedhumanembryonicstemcell-derivedpancreaticendocrineisletcells.
CellProlif.
2008;41:843–58.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page16of1914.
KroonE,MartinsonLA,KadoyaK,etal.
Pancreaticendodermderivedfromhumanembryonicstemcellsgeneratesglucose-responsiveinsulin-secretingcellsinvivo.
NatBiotechnol.
2008;26:443–52.
15.
ChenS,BorowiakM,FoxJL,etal.
AsmallmoleculethatdirectsdifferentiationofhumanESCsintothepancreaticlineage.
NatChemBiol.
2009;5:258–65.
16.
ZhangD,JiangW,LiuM,etal.
HighlyefficientdifferentiationofhumanEScellsandiPScellsintomaturepancreaticinsulin-producingcells.
CellRes.
2009;19:429–38.
17.
KunisadaY,Tsubooka-YamazoeN,ShojiM,etal.
Smallmoleculesinduceefficientdifferentiationintoinsulin-producingcellsfromhumaninducedpluripotentstemcells.
StemCellRes.
2012;8:274–84.
18.
RezaniaA,BruinJE,RiedelMJ,etal.
Maturationofhumanembryonicstemcell-derivedpancreaticprogenitorsintofunctionalisletscapableoftreatingpre-existingdiabetesinmice.
Diabetes.
2012;61:2016–29.
19.
SchulzTC,YoungHY,AgulnickAD,etal.
Ascalablesystemforproductionoffunctionalpancreaticprogenitorsfromhumanembryonicstemcells.
PLoSOne.
2012;7:e37004.
20.
BruinJE,RezaniaA,XuJ,etal.
Maturationandfunctionofhumanembryonicstemcell-derivedpancreaticprogenitorsinmacroencapsulationdevicesfollowingtransplantintomice.
Diabetologia.
2013;56:1987–98.
21.
RezaniaA,BruinJE,XuJ,etal.
Enrichmentofhumanembryonicstemcell-derivedNKX6.
1-expressingpancreaticprogenitorcellsacceleratesthematurationofinsulin-secretingcellsinvivo.
StemCells.
2013;31:2432–42.
22.
RezaniaA,BruinJE,AroraP,etal.
Reversalofdiabeteswithinsulin-producingcellsderivedinvitrofromhumanpluripotentstemcells.
NatBiotechnol.
2014;32:1121–33.
23.
PagliucaFW,MillmanJR,GurtlerM,etal.
Generationoffunctionalhumanpancreaticβcellsinvitro.
Cell.
2014;159:428–39.
24.
ShahjalalHM,ShirakiN,SakanoD,etal.
Generationofinsulin-producingbeta-likecellsfromhumaniPScellsinadefinedandcompletelyxeno-freeculturesystem.
JMolCellBiol.
2014;6:394–408.
25.
AgulnickAD,AmbruzsDM,MoormanMA,etal.
Insulin-producingendocrinecellsdifferentiatedinvitrofromhumanembryonicstemcellsfunctioninmacroencapsulationdevicesinvivo.
StemCellsTranslMed.
2015;4:1214–22.
26.
ToyodaT,MaeS-I,TanakaH,etal.
CellaggregationoptimizesthedifferentiationofhumanESCsandiPSCsintopancreaticbud-likeprogenitorcells.
StemCellRes.
2015;14:185–97.
27.
MillmanJR,XieC,DervortAV,etal.
Generationofstemcell-derivedβ-cellsfrompatientswithtype1diabetes.
NatCommun.
2016;7:11463.
28.
ManzarGS,KimEM,ZavazavaN,etal.
Demethylationofinducedpluripotentstemcellsfromtype1diabeticpatientsenhancesdifferentiationintofunctionalpancreaticβ-cells.
JBiolChem.
2017;292:14066–79.
29.
YabeSG,FukudaS,TakedaF,etal.
Efficientgenerationoffunctionalpancreaticβ-cellsfromhumaninducedpluripotentstemcells.
JDiabetes.
2017;9:168–79.
30.
NostroMC,SarangiF,OgawaS,etal.
Stage-specificsignalingthroughTGFβfamilymembersandWNTregulatespatterningandpancreaticspecificationofhumanpluripotentstemcells.
Development.
2011;138:861–71.
31.
XuX,BrowningVL,OdoricoJS.
Activin,BMPandFGFpathwayscooperatetopromoteendodermandpancreaticlineagecelldifferentiationfromhumanembryonicstemcells.
MechDev.
2011;128:412–27.
32.
BruinJE,ErenerS,VelaJ,etal.
Characterizationofpolyhormonalinsulin-producingcellsderivedinvitrofromhumanembryonicstemcells.
StemCellRes.
2014;12:194–208.
33.
BasfordCL,PrenticeKJ,HardyAB,etal.
Thefunctionalandmolecularcharacterisationofhumanembryonicstemcell-derivedinsulin-positivecellscomparedwithadultpancreaticbetacells.
Diabetologia.
2012;55:358–71.
34.
GuoS,DaiC,GuoM,etal.
Inactivationofspecificβcelltranscriptionfactorsintype2diabetes.
JClinInvest.
2013;123:3305–16.
35.
KirkK,HaoE,LahmyR,etal.
Humanembryonicstemcellderivedisletprogenitorsmatureinsideanencapsulationdevicewithoutevidenceofincreasedbiomassorcellescape.
StemCellRes.
2014;12:807–14.
36.
ClinicalTrials.
govIdentifier:NCT02239354.
ViaCyte,Inc.
,SanDiego,CA.
http://viacyte.
com/clinical/clinical-trials.
37.
ThomsonJA,Itskovitz-EldorJ,ShapiroSS,etal.
Embryonicstemcelllinesderivedfromhumanblastocysts.
Science.
1998;282:1145–7.
38.
ReubinoffBE,PeraMF,FongCY,etal.
Embryonicstemcelllinesfromhumanblastocysts:somaticdifferentiationinvitro.
NatBiotechnol.
2000;18:399–404.
39.
CowanCA,KlimanskayaI,McMahonJ,etal.
Derivationofembryonicstem-celllinesfromhumanblastocysts.
NEnglJMed.
2004;350:1353–6.
40.
TakahashiK,YamanakaS.
Inductionofpluripotentstemcellsfrommouseembryonicandadultfibroblastculturesbydefinedfactors.
Cell.
2006;126:663–76.
41.
TakahashiK,TanabeK,OhnukiM,etal.
Inductionofpluripotentstemcellsfromadulthumanfibroblastsbydefinedfactors.
Cell.
2007;131:861–72.
42.
YuJ,VodyanikMA,Smuga-OttoK,etal.
Inducedpluripotentstemcelllinesderivedfromhumansomaticcells.
Science.
2007;318:1917–20.
43.
MaheraliN,HochedlingerK.
Guidelinesandtechniquesforthegenerationofinducedpluripotentstemcells.
CellStemCell.
2008;3:595–605.
44.
FedericoG,BouéS,BelmonteJCI.
Methodsformakinginducedpluripotentstemcells:reprogrammingalacarte.
NatRevGenet.
2011;12:231–42.
45.
O'DohertyR,GreiserU,WangW.
Nonviralmethodsforinducingpluripotencytocells.
BiomedResInt.
2013;2013:705902.
46.
MalikN,RaoMS.
AreviewofthemethodsforhumaniPSCderivation.
MethodsMolBiol.
2013;997:23–33.
47.
ZhouYY,ZengF.
Integration-freemethodsforgeneratinginducedpluripotentstemcells.
GenomicsProteomicsBioinformatics.
2013;11:284–7.
48.
NarayananK,MishraS,SinghS,etal.
Engineeringconceptsinstemcellresearch.
BiotechnolJ.
2017;12:1700066.
49.
MatsuiT,LeungD,MiyashitaH,etal.
ProviralsilencinginembryonicstemcellsrequiresthehistonemethyltransferaseESET.
Nature.
2010;464:927–31.
50.
KimD,KimCH,MoonJI,etal.
Generationofhumaninducedpluripotentstemcellsbydirectdeliveryofreprogrammingproteins.
CellStemCell.
2009;4:472–6.
51.
WoltjenK,MichaelIP,MohseniP,etal.
piggyBactranspositionreprogramsfibroblaststoinducedpluripotentstemcells.
Nature.
2009;458:766–70.
52.
YuJ,HuK,Smuga-OttoK,etal.
Humaninducedpluripotentstemcellsfreeofvectorandtransgenesequences.
Science.
2009;324:797–801.
53.
JiaF,WilsonKD,SunN,etal.
AnonviralminicirclevectorforderivinghumaniPScells.
NatMethods.
2010;7:197–9.
54.
WarrenL,ManosPD,AhfeldtT,etal.
HighlyefficientreprogrammingtopluripotencyanddirecteddifferentiationofhumancellsusingsyntheticmodifiedmRNA.
CellStemCell.
2010;7:618–30.
55.
LeeCH,KimJ-H,LeeHJ,etal.
ThegenerationofiPScellsusingnon-viralmagneticnanoparticlebasedtransfection.
Biomaterials.
2011;32:6683–91.
56.
OkitaK,MatsumuraY,SatoY,etal.
Amoreefficientmethodtogenerateintegration-freehumaniPScells.
NatMethods.
2011;8:409–12.
57.
ChoiHY,LeeT-J,YangG-M,etal.
EfficientmRNAdeliverywithgrapheneoxide-polyethylenimineforgenerationoffootprint-freehumaninducedpluripotentstemcells.
JControlRelease.
2016;235:222–35.
58.
ChinMH,MasonMJ,XieW,etal.
Inducedpluripotentstemcellsandembryonicstemcellsaredistinguishedbygeneexpressionsignatures.
CellStemCell.
2009;5:111–23.
59.
DoiA,ParkIH,WenB,etal.
Differentialmethylationoftissue-andcancer-specificCpGislandshoresdistinguisheshumaninducedpluripotentstemcells,embryonicstemcellsandfibroblasts.
NatGenet.
2009;41:1350–3.
60.
MaysharY,Ben-DavidU,LavonN,etal.
Identificationandclassificationofchromosomalaberrationsinhumaninducedpluripotentstemcells.
CellStemCell.
2010;7:521–31.
61.
PickM,StelzerY,Bar-NurO,etal.
Clone-andgene-specificaberrationsofparentalimprintinginhumaninducedpluripotentstemcells.
StemCells.
2009;27:2686–90.
62.
FengQ,LuSJ,KlimanskayaI,etal.
Hemangioblasticderivativesfromhumaninducedpluripotentstemcellsexhibitlimitedexpansionandearlysenescence.
StemCells.
2010;28:704–12.
63.
HuB-Y,WeickJP,YuJ,etal.
Neuraldifferentiationofhumaninducedpluripotentstemcellsfollowsdevelopmentalprinciplesbutwithvariablepotency.
ProcNatlAcadSci.
2010;107:4335–40.
64.
UrbachA,Bar-NurO,DaleyGQ,etal.
DifferentialmodelingoffragileXsyndromebyhumanembryonicstemcellsandinducedpluripotentstemcells.
CellStemCell.
2010;6:407–11.
65.
MiuraK,OkadaY,AoiT,etal.
Variationinthesafetyofinducedpluripotentstemcelllines.
NatBiotechnol.
2009;27:743–5.
66.
AssadyS,MaorG,AmitM,etal.
Insulinproductionbyhumanembryonicstemcells.
Diabetes.
2001;50:1691–7.
67.
Aguayo-MazzucatoC,ZavackiAM,MarinelarenaA,etal.
Thyroidhormonepromotespostnatalratpancreaticβ-celldevelopmentandglucose-responsiveinsulinsecretionthroughMAFA.
Diabetes.
2013;62:1569–80.
68.
MemonB,KaramM,Al-KhawagaS,etal.
Enhanceddifferentiationofhumanpluripotentstemcellsintopancreaticprogenitorsco-expressingPDX1andNKX6.
1.
StemCellResTher.
2018;9:15.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page17of1969.
NostroMC,SarangiF,YangC,etal.
EfficientgenerationofNKX6-1+pancreaticprogenitorsfrommultiplehumanpluripotentstemcelllines.
StemCellRep.
2015;4:591–604.
70.
deKrijgerRR,AanstootHJ,KranenburgG,etal.
Themidgestationalhumanfetalpancreascontainscellscoexpressingislethormones.
DevBiol.
1992;153:368–75.
71.
HrvatinS,O'DonnellCW,DengF,etal.
Differentiatedhumanstemcellsresemblefetal,notadult,βcells.
ProcNatlAcadSci.
2014;111:3038–43.
72.
RiedelMJ,AsadiA,WangR,etal.
Immunohistochemicalcharacterisationofcellsco-producinginsulinandglucagoninthedevelopinghumanpancreas.
Diabetologia.
2012;55:372–81.
73.
KellyOG,ChanMY,MartinsonLA,etal.
Cell-surfacemarkersfortheisolationofpancreaticcelltypesderivedfromhumanembryonicstemcells.
NatBiotechnol.
2011;29:750–6.
74.
XieR,EverettLJ,LimH-W,etal.
Dynamicchromatinremodelingmediatedbypolycombproteinsorchestratespancreaticdifferentiationofhumanembryonicstemcells.
CellStemCell.
2013;12:224–37.
75.
RojasA,KhooA,TejedoJR,etal.
Isletcelldevelopment.
AdvExpMedBiol.
2010;654:59–75.
76.
SeymourPA,SanderM.
Historicalperspective:beginningsoftheβ-cell:currentperspectivesinβ-celldevelopment.
Diabetes.
2011;60:364–76.
77.
ArdaHE,BenitezCM,KimSK,etal.
Generegulatorynetworksgoverningpancreasdevelopment.
DevCell.
2013;25:5–13.
78.
RorsmanP,BraunM.
Regulationofinsulinsecretioninhumanpancreaticislets.
AnnuRevPhysiol.
2013;75:155–79.
79.
BenningerRKP,PistonDW.
Cellularcommunicationandheterogeneityinpancreaticisletinsulinsecretiondynamics.
TrendsEndocrinolMetab.
2014;25:399–406.
80.
PeirisH,BonderCS,CoatesPT,etal.
Theβ-cell/ECaxis:howdoisletcellstalktoeachotherDiabetes.
2014;63:3–11.
81.
WangW,JinS,YeK,etal.
DevelopmentofisletorganoidsfromH9humanembryonicstemcellsinbiomimetic3Dscaffolds.
StemCellsDev.
2017;26:394–404.
82.
CandielloJ,PavanGrandhiTS,GohSK,etal.
3Dheterogeneousisletorganoidgenerationfromhumanembryonicstemcellsusinganovelengineeredhydrogelplatform.
Biomaterials.
2018;177:27–39.
83.
JiangJ,AuM,LuK,etal.
Generationofinsulin-producingislet-likeclustersfromhumanembryonicstemcells.
StemCells.
2007;25:1940–53.
84.
TateishiK,HeJ,TaranovaO,etal.
Generationofinsulin-secretingislet-likeclustersfromhumanskinfibroblasts.
JBiolChem.
2008;283:31601–7.
85.
ShimJH,KimJ,HanJ,etal.
Pancreaticislet-likethree-dimensionalaggregatesderivedfromhumanembryonicstemcellsamelioratehyperglycemiainstreptozotocin-induceddiabeticmice.
CellTransplant.
2015;24:2155–68.
86.
KimY,KimH,KoUH,etal.
Islet-likeorganoidsderivedfromhumanpluripotentstemcellsefficientlyfunctionintheglucoseresponsivenessinvitroandinvivo.
SciRep.
2016;6:35145.
87.
TakahashiY,SekineK,KinT,etal.
Self-condensationcultureenablesvascularizationoftissuefragmentsforefficienttherapeutictransplantation.
CellRep.
2018;23:1620–9.
88.
HickmanGJ,BoocockDJ,PockleyAG,etal.
Theimportanceandclinicalrelevanceofsurfacesintissueculture.
ACSBiomaterSciEng.
2016;2:152–64.
89.
WaltersNJ,GentlemanE.
Evolvinginsightsincell-matrixinteractions:elucidatinghownon-solublepropertiesoftheextracellularnichedirectstemcellfate.
ActaBiomater.
2015;11:3–16.
90.
BakerLA,TiriacH,CleversH,etal.
Modelingpancreaticcancerwithorganoids.
TrendsCancer.
2016;2:176–90.
91.
YinX,MeadBE,SafaeeH,etal.
Engineeringstemcellorganoids.
CellStemCell.
2016;18:25–38.
92.
GieniRS,HendzelMJ.
MechanotransductionfromtheECMtothegenome:arethepiecesnowinplaceJCellBiochem.
2008;104:1964–87.
93.
ThomasD,O'BrienT,PanditA.
Towardcustomizedextracellularnicheengineering:progressincell-entrapmenttechnologies.
AdvMater.
2018;30:1703948.
94.
SchuppinGT,Bonner-WeirS,MontanaE,etal.
Replicationofadultpancreatic-betacellsculturedonbovinecornealendothelialcellextracellularmatrix.
InVitroCellDevBiolAnim.
1993;29A:339–44.
95.
BoscoD,MedaP,HalbanPA,etal.
Importanceofcell-matrixinteractionsinratisletbeta-cellsecretioninvitro:roleofalpha6beta1integrin.
Diabetes.
2000;49:233–43.
96.
WeberLM,HaydaKN,AnsethKS,etal.
Cell-matrixinteractionsimprovebeta-cellsurvivalandinsulinsecretioninthree-dimensionalculture.
TissueEngPartA.
2008;14:1959–68.
97.
RisF,HammarE,BoscoD,etal.
Impactofintegrin-matrixmatchingandinhibitionofapoptosisonthesurvivalofpurifiedhumanbeta-cellsinvitro.
Diabetologia.
2002;45:841–50.
98.
HammarE,ParnaudG,BoscoD,etal.
Extracellularmatrixprotectspancreaticβ-cellsagainstapoptosis:roleofshort-andlong-termsignalingpathways.
Diabetes.
2004;53:2034–41.
99.
LeeJH,YuHS,LeeGS,etal.
Collagengelthree-dimensionalmatricescombinedwithadhesiveproteinsstimulateneuronaldifferentiationofmesenchymalstemcells.
JRSocInterface.
2011;8:998–1010.
100.
ZimmermannWH,SchneiderbangerK,SchubertP,etal.
Tissueengineeringofadifferentiatedcardiacmuscleconstruct.
CircRes.
2002;90:223–30.
101.
LuS-H,WangH-B,LiuH,etal.
Reconstructionofengineereduterinetissuescontainingsmoothmusclelayerincollagen/Matrigelscaffoldinvitro.
TissueEngPartA.
2009;15:1611–8.
102.
LiW,ZhaoR,LiuJ,etal.
Smallisletstransplantationsuperioritytolargeones:implicationsfromisletmicrocirculationandrevascularization.
JDiabetesRes.
2014;2014:192093.
103.
TakebeT,EnomuraM,YoshizawaE,etal.
Vascularizedandcomplexorganbudsfromdiversetissuesviamesenchymalcell-drivencondensation.
CellStemCell.
2015;16:556–65.
104.
LancasterMA,KnoblichJA.
Organogenesisinadish:modelingdevelopmentanddiseaseusingorganoidtechnologies.
Science.
2014;345:1247125.
105.
TakahashiY,TakebeT,TaniguchiH,etal.
Engineeringpancreatictissuesfromstemcellstowardstherapy.
RegenTher.
2016;3:15–23.
106.
YanagawaF,KajiH,JangY-H,etal.
Directedassemblyofcell-ladenmicrogelsforbuildingporousthree-dimensionaltissueconstructs.
JBiomedMaterResA.
2011;97:93–102.
107.
KharkarPM,KiickKL,KloxinAM.
Designingdegradablehydrogelsfororthogonalcontrolofcellmicroenvironments.
ChemSocRev.
2013;42:7335–72.
108.
StendahlJC,KaufmanDB,StuppSI.
Extracellularmatrixinpancreaticislets:relevancetoscaffolddesignandtransplantation.
CellTransplant.
2009;18:1–12.
109.
DudleyAC.
Tumorendothelialcells.
ColdSpringHarbPerspectMed.
2012;2:a006536.
110.
KreutzigerKL,MuskheliV,JohnsonP,etal.
Developingvasculatureandstromainengineeredhumanmyocardium.
TissueEngPartA.
2011;17:1219–28.
111.
OkitaK,IchisakaT,YamanakaS.
Generationofgermline-competentinducedpluripotentstemcells.
Nature.
2007;448:313–7.
112.
NakagawaM,KoyanagiM,TanabeK,etal.
GenerationofinducedpluripotentstemcellswithoutMycfrommouseandhumanfibroblasts.
NatBiotechnol.
2008;26:101–6.
113.
Hacein-Bey-AbinaS,VonKalleC,SchmidtM,etal.
LMO2-associatedclonalTcellproliferationintwopatientsaftergenetherapyforSCID-X1.
Science.
2003;302:415–9.
114.
StadtfeldM,NagayaM,UtikalJ,etal.
Inducedpluripotentstemcellsgeneratedwithoutviralintegration.
Science.
2008;322:945–9.
115.
ZhouW,FreedCR.
Adenoviralgenedeliverycanreprogramhumanfibroblaststoinducedpluripotentstemcells.
StemCells.
2009;27:2667–74.
116.
FusakiN,BanH,NishiyamaA,etal.
Efficientinductionoftransgene-freehumanpluripotentstemcellsusingavectorbasedonSendaivirus,anRNAvirusthatdoesnotintegrateintothehostgenome.
ProcJapanAcadSerB.
2009;85:348–62.
117.
OkitaK,YamanakaS.
Inductionofpluripotencybydefinedfactors.
ExpCellRes.
2010;316:2565–70.
118.
OsafuneK,CaronL,BorowiakM,etal.
Markeddifferencesindifferentiationpropensityamonghumanembryonicstemcelllines.
NatBiotechnol.
2008;26:313–5.
119.
CoboF,StaceyG,HuntC,etal.
Microbiologicalcontrolinstemcellbanks:approachestostandardisation.
ApplMicrobiolBiotechnol.
2005;68:456–66.
120.
MartinMJ,MuotriA,GageF,etal.
Humanembryonicstemcellsexpressanimmunogenicnonhumansialicacid.
NatMed.
2005;11:228–32.
121.
SkottmanH,HovattaO.
Cultureconditionsforhumanembryonicstemcells.
Reproduction.
2006;132:691–8.
122.
MicallefSJ,LiX,SchiesserJV,etal.
INSGFP/whumanembryonicstemcellsfacilitateisolationofinvitroderivedinsulin-producingcells.
Diabetologia.
2012;55:694–706.
123.
YoshiharaE,WeiZ,LinCS,etal.
ERRγisrequiredforthemetabolicmaturationoftherapeuticallyfunctionalglucose-responsiveβcells.
CellMetab.
2016;23:622–34.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page18of19124.
SaberN,BruinJE,O'DwyerS,etal.
Sexdifferencesinmaturationofhumanembryonicstemcell-derivedβcellsinmice.
Endocrinology.
2018;159:1827–41.
125.
SchuitF,VanLommelL,GranvikM,etal.
β-cell–specificgenerepression:amechanismtoprotectagainstinappropriateormaladjustedinsulinsecretionDiabetes.
2012;61:969–75.
126.
PepperAR,Gala-LopezB,PawlickR,etal.
Aprevascularizedsubcutaneousdevice-lesssiteforisletandcellulartransplantation.
NatBiotechnol.
2015;33:518–23.
127.
VegasAJ,VeisehO,GurtlerM,etal.
Long-termglycemiccontrolusingpolymerencapsulatedhumanstem-cellderivedβ-cellsinimmunecompetentmice.
NatMed.
2016;22:306–11.
128.
WeirGC.
Isletencapsulation:advancesandobstacles.
Diabetologia.
2013;56:1458–61.
129.
HermannM,PirkebnerD,DraxlA,etal.
Dickkopf-3isexpressedinasubsetofadulthumanpancreaticbetacells.
HistochemCellBiol.
2007;127:513–21.
130.
SaishoY,HarrisPE,ButlerAE,etal.
Relationshipbetweenpancreaticvesicularmonoaminetransporter2(VMAT2)andinsulinexpressioninhumanpancreas.
JMolHistol.
2008;39:543–51.
131.
DorrellC,SchugJ,CanadayPS,etal.
Humanisletscontainfourdistinctsubtypesofβcells.
NatCommun.
2016;7:11756.
132.
WallisRH,WangK,MarandiL,etal.
Type1diabetesintheBBrat:apolygenicdisease.
Diabetes.
2009;58:1007–17.
133.
ZhangW,KamiyaH,EkbergK,etal.
C-peptideimprovesneuropathyintype1diabeticBB/Wor-rats.
DiabetesMetabResRev.
2007;23:63–70.
134.
vonHerrathM,FilippiC,CoppietersK.
Howviralinfectionsenhanceorpreventtype1diabetes-frommousetoman.
JMedVirol.
2011;83:1672.
135.
MullerYD,GolshayanD,EhirchiouD,etal.
Immunosuppressiveeffectsofstreptozotocin-induceddiabetesresultinabsolutelymphopeniaandarelativeincreaseofT-regulatorycells.
Diabetes.
2011;60:2331–40.
136.
BrosiusFC,AlpersCE,BottingerEP,etal.
Mousemodelsofdiabeticnephropathy.
JAmSocNephrol.
2009;20:2503–12.
137.
GageBK,WebberTD,KiefferTJ.
Initialcellseedingdensityinfluencespancreaticendocrinedevelopmentduringinvitrodifferentiationofhumanembryonicstemcells.
PLoSOne.
2013;8:e82076.
138.
RazaA,ChangSK,LinCC.
Theinfluenceofmatrixpropertiesongrowthandmorphogenesisofhumanpancreaticductalepithelialcellsin3D.
Biomaterials.
2013;34:5117–27.
139.
ShihHP,PanlasiguiD,CirulliV,etal.
ECMsignalingregulatescollectivecellulardynamicstocontrolpancreasbranchingmorphogenesis.
CellRep.
2016;14:169–79.
140.
SneddonJB,TangQ,StockP,etal.
Stemcelltherapiesfortreatingdiabetes:progressandremainingchallenges.
CellStemCell.
2018;22:810–23.
Shahjalaletal.
StemCellResearch&Therapy(2018)9:355Page19of19
- resultantesetnod32id相关文档
- pantaesetnod32id
- stuckesetnod32id
- alarmsesetnod32id
- Examplesesetnod32id
- Useresetnod32id
- staresetnod32id
DMIT$10.9/月,日本VPS/三网直连/1核1.5G内存/20GB存储/1Gbps端口
优惠码年付一次性5折优惠码:TYO-Lite-Open-Beta-1y-50OFF永久8折优惠码:TYO-Lite-Open-Beta-Recur-20OFF日本vpsCPU内存SSD流量带宽价格购买1核1.5G20 GB4 TB1Gbps$10.9/月购买2核2 G40 GB6 TB1Gbps$16.9/月购买2核4 G60 GB8 TB1Gbps$21.9/月购买4核4 G80 GB12 TB...
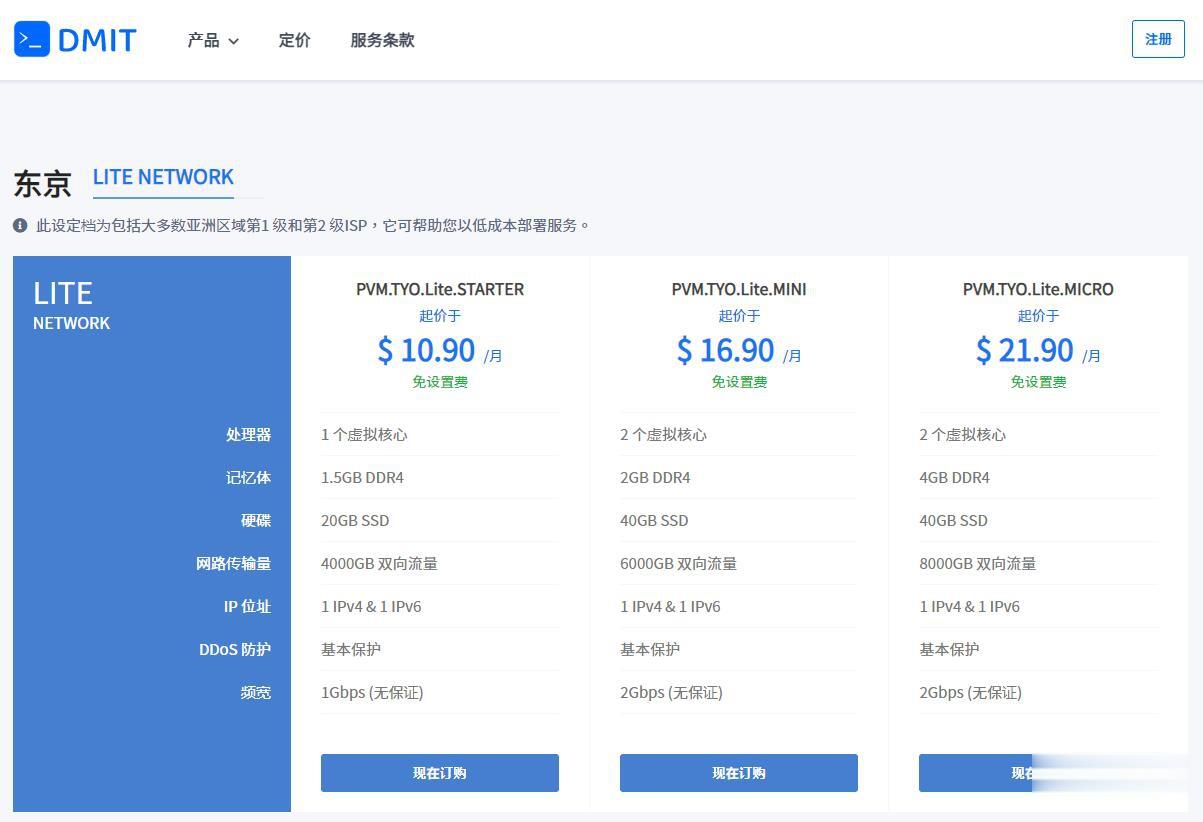
ParkInHost - 俄罗斯VPS主机 抗投诉 55折,月付2.75欧元起
ParkInHost主机商是首次介绍到的主机商,这个商家是2013年的印度主机商,隶属于印度DiggDigital公司,主营业务有俄罗斯、荷兰、德国等机房的抗投诉虚拟主机、VPS主机和独立服务器。也看到商家的数据中心还有中国香港和美国、法国等,不过香港机房肯定不是直连的。根据曾经对于抗投诉外贸主机的了解,虽然ParkInHost以无视DMCA的抗投诉VPS和抗投诉服务器,但是,我们还是要做好数据备...

华纳云,3折低至优惠云服务器,独立服务器/高防御服务器低至6折,免备案香港云服务器CN2 GIA三网直连线路月付18元起,10Mbps带宽不限流量
近日华纳云发布了最新的618返场优惠活动,主要针对旗下的免备案香港云服务器、香港独立服务器、香港高防御服务器等产品,月付6折优惠起,高防御服务器可提供20G DDOS防御,采用E5处理器V4CPU性能,10Mbps独享CN2 GIA高速优质带宽,有需要免备案香港服务器、香港云服务器、香港独立服务器、香港高防御服务器、香港物理服务器的朋友可以尝试一下。华纳云好不好?华纳云怎么样?华纳云服务器怎么样?...
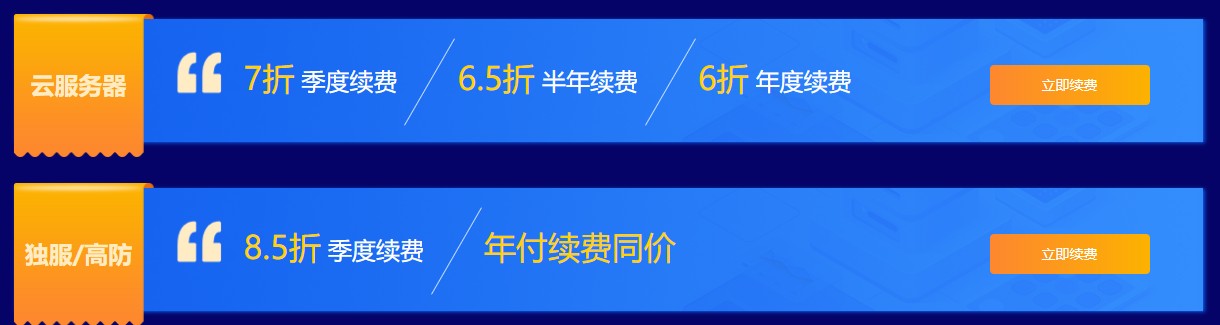
esetnod32id为你推荐
-
generatedgoogleIntentsandroid支持ipadx-router设置路由器是我的上网设置是x怎么弄谷歌sb为什么百度一搜SB是谷歌,谷歌一搜SB是百度?chromeframe无法安装chrome frame,求助googleadsenceGoogle AdSense 帐户状态是什么意思!迅雷雷鸟100+怒放手机是迅雷做的么?迅雷之前不是出了一款雷鸟手机么?www.baidu.jp日本视频怎样看chrome18怎么关闭chrome的自动更新,稳定版要18了,mactype要悲剧了