tests38ab.com
38ab.com 时间:2021-03-21 阅读:()
RESEARCHARTICLEOpenAccessPerspectivesontheimpactofpainfuldiabeticperipheralneuropathyinamulticulturalpopulationMartinEichholz1,AndreaH.
Alexander2,JosephC.
Cappelleri3,PatrickHlavacek2,BruceParsons2,AlesiaSadosky2*andMichaelM.
Tuchman4AbstractBackground:Sincefewstudieshavecharacterizedpainfuldiabeticperipheralneuropathy(pDPN)symptomsinmulticulturalpopulations,thisstudyfieldedasurveytobetterunderstandpDPNanditsimpactinAfrican-American,Caucasian,andHispanicpopulations.
Methods:KeltonfieldedasurveybyphoneorInternet,inEnglishorSpanish,amongadultswithpDPNsymptomsintheUnitedStatesbetweenAugustandOctober2015;African-AmericansandHispanicswereoversampledtoachieveatleast500subjectsforeachgroup.
PatientswererequiredtohavebeendiagnosedwithpDPNorscore≥3onIDPainvalidatedscreeningtool.
ThesurveyelicitedinformationonpDPNsymptomsandinteractionswithhealthcareproviders(HCPs),andincludedtheBriefPainInventoryandpain-specificWorkProductivityandAssessmentQuestionnaire(WPAI:SHP).
Results:Respondentsincluded823Caucasians,525African-Americans,and537Hispanics;approximatelyhalfofAfrican-AmericansandHispanicswere<40yearsofage,vs12%ofCaucasians.
PainwaslesslikelytoberatedmoderateorseverebyAfrican-Americans(65%)andHispanics(49%)relativetoCaucasians(87%;p<0.
05).
African-AmericansandHispanicswerelesslikelythanCaucasianstoreportexperiencingspecificpDPNsensorysymptoms.
SignificantlyfewerAfrican-AmericansandHispanicsreportedreceivingapDPNdiagnosisrelativetoCaucasians(p<0.
05),andhigherproportionsofAfrican-AmericansandHispanicsreporteddifficultycommunicatingwiththeirHCP(p<0.
05).
WPAI:SHPactivityimpairmentwaslowerinHispanics(43%)relativetoAfrican-Americans(53%)andCaucasian(56%;p<0.
05).
Conclusions:MulticulturalpatientsreporteddifferencesinpDPNsymptomsandpainrelativetoCaucasians,andfewerreceivedapDPNdiagnosis.
Whilefurtherevaluationisneededtounderstandthesedifferences,thesedatasuggestaneedtobroadenpDPNeducationalinitiativestoimprovepatient-HCPdialogueandencouragediscussionofpDPNsymptomsandtheirimpactinamulticulturalsetting.
Keywords:Painfuldiabeticperipheralneuropathy,Race,Ethnicity,Pain,Productivity*Correspondence:Alesia.
sadosky@pfizer.
com2PfizerInc.
,235East42ndStreet,NewYork,NY10017,USAFulllistofauthorinformationisavailableattheendofthearticleTheAuthor(s).
2017OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12DOI10.
1186/s40842-017-0051-2BackgroundDiabeticperipheralneuropathy(DPN)isacommoncomplicationofType1andType2diabetesthatischaracterizedbynervedamage.
WhenDPNpresentswithpainfulsymptomstheconditionisknownaspainfuldiabeticperipheralneuropathy(pDPN).
Whiletheepi-demiologyofpDPNhasnotbeenwell-characterized,anoverallprevalenceof15%hasbeenestimatedinthedia-beticpopulation[1].
However,prevalenceratesexceed-ing30%inpatientswithdiabeteshavebeenreportedinmorerecentregionalstudies[2,3],andasystematicreviewofneuropathicpaininthegeneralpopulationreportedapDPNprevalenceof0.
8%thatrepresentsapproximately26%ofindividualswithType2diabetes[4].
Thesubstantialpatientandeconomicburdensassoci-atedwithpDPNarewell-recognizedandincludereduc-tionsinpatientfunction,qualityoflife,andproductivity[5,6],aswellasgreaterhealthcareresourceutilizationandcostsrelativetopatientswithdiabetesandwithDPNwithoutpain[7].
Despitestudiesevaluatingqualityoflifeandotherpatient-reportedoutcomesinpDPN,therearelimiteddataontheseverityandimpactofpainfulpDPNsymp-tomsfromthepatient'sperspective.
Asurveyinpatientsandclinicianswhotreatpatientswithdiabetesnotonlyshowedthatmisperceptionsonthecauseandmanage-mentofpDPNwerecommoninbothstakeholdergroupsbutalsoindicatedadditionaldisparitiesbetweenpatientandclinicianperspectivesregardingcommunica-tion,severity,andtreatment[8].
However,lessisknownaboutthepatientperceptionsofpDPNandinteractionsbetweenthesepatientsandtheirhealthcareproviders(HCPs)inamulticulturalpopulation.
Therefore,theobjectiveofthisstudywastocharacterizetheimpactofpDPNandidentifybarrierstoitsmanagementinamulticulturalUSpopulationwithafocusonAfrican-AmericansandHispanicsrelativetoCaucasians.
MethodsDesignandpopulationsKeltonfieldedasurveyamongpDPNpatientsintheUnitedStatesbetweenAugustandOctober2015.
Forinclusion,patientswererequiredtobeadults(≥18yearsold)whoself-reportedbeingdiagnosedwitheitherType1orType2diabetesandeitherself-reportedhavingreceivedadiagnosisofpDPNbyanHCPorhadascore≥3onIDPain[9](i.
e.
,experienced≥3ofthefollowingsymptomswithinthepastweek:pinsandneedles,hot/burning,numbness,electricalshocks,orpainthatismadeworsewiththetouchofclothingorbedsheets).
IDPainisavalidatedmeasurethatisusedtoscreenpatientsforthepresenceofneuropathicpainbasedonitsdemonstratedabilitytodiscriminatebetweennociceptiveandneuropathicpain[9].
Thesurvey,whichwasdevelopedwithoutpatientinputbutincollaborationwithexpertsinthefield,includingclinicians,wasadministeredbyInternetamongCaucasians,andbyeitherInternetorphoneamongAfrican-AmericansandHispanics,withInternetrespondentsrecruitedfromanationalresearchpanelandphonerespondentsrecruitedfrompurchasedphonelists.
Oversamplingviaphonewasperformedtoachieveagoalofatleast500Hispanicpatientsand500African-Americanpatients.
ThesurveycouldbecompletedinEnglishorSpanish,withtheSpanishversionback-translatedbynativeSpanish-speakerstoensureaccuracyofthequestionnaire.
Thesurvey(Additionalfile1)consistedofbatteriesofquestionsthatwereinpartderivedfromaprevious,simi-larsurvey[8].
ThegoalwastocaptureperspectivesonpDPNsymptoms(numbness;pinsandneedles;painordiscomfortatnight;tinglingorpricklingsensation;sensi-tivitytotouch;burningpainorsensation;shootingpain;radiatingpain;stinging;stabbingpain;electricshock-likesymptomsorsuddenpainattacks;throbbingpain),perceptionsofpainassociatedwiththesymptoms,andhowpatientsdiscussthesesymptomswiththeirphysician.
Additionally,thesurveyincludedtheBriefPainInven-tory(BPI)[10]andtheWorkProductivityandAssessmentQuestionnairedisease-specificversion(WPAI:SHP)adaptedforpain[11],bothofwhichdemonstratesoundpsychometricmeasurementpropertiesandhavebeenusedasoutcomesacrossawidevarietyofdiseasestates.
TheBPIratesworst,least,andaveragepaininthepast24handtheaveragepainsubscalewasusedtocategorizepainasmild,moderate,andseverebasedonestablishedcutpointsfortheaveragepainscaleof0–3formild,4–6formoderate,and7–10forsevere[12].
TheWPAI:SHPmeasuresimpactofthediseaseonproductivityatworkduetoabsenteeism(worktimemissed),presenteeism(impairmentwhileatwork),overallworkimpairment,andactivityimpairmentoutsideofworkduringthepast7days.
StatisticalanalysisSurveyresultsreflectanunweightedsample.
Themarginoferrorwas±3.
1%forthetotalpatientsampleand4.
0%fortheoversampledgroups.
Analysesforcategoricaldataandcontinuousdatawereconductedusingchi-squaretestsandt-tests,respectively.
Theimpactofethnicitywasexploredbasedonthecombinedmainsampleandover-sampleandcontrolledforeffectsofage,education,andhouseholdincomeusinglayeredcross-tabulations(chi-squaretests)andstepwiselinearregression[13].
Thecross-tabulationswereconductedusing16demographicstrata:3agegroups(18–34years,35–54years,and≥55years),6educationlevels,and7incomelevelsshowninthedemographicstable(Table1).
Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page2of9Stepwiselinearregressionwasalsoperformedamongthemainsample,usingpainseverityasthedependentvariableand10itemsrelatedtothepatients'experiencewithsymptomsasindependentvariables(numbness;pinsandneedles;painordiscomfortatnight;tinglingorpricklingsensation;sensitivitytotouch;burningpainorsensation;shootingpain;stinging;stabbingpain;electricshock-likesymptomsorsuddenpainattacks).
AllanalyseswereperformedusingIBMSPSSStatistics23.
ResultsRespondentpopulationsTable1presentsthedemographiccharacteristicsofthemulticulturalpopulations,andshowsthatmeanagewassignificantlyhigher(p<0.
05)amongCaucasiansthanAfrican-AmericansandHispanics,anddifferenceswerealsoobservedintheagedistribution.
AlmosthalfoftheAfrican-Americans(49%)andmorethanhalfoftheHis-panics(59%)wereunder40yearsofage,comparedwithonly12%ofCaucasians.
Caucasianshadthelowestrateofemploymentandthehighestrateofretireesamongthethreeculturalgroups,andannualincomewashigh-estinHispanics,lowestamongCaucasians.
Consistentwiththeolderdemographic,asignificantlygreaterpro-portionofCaucasiansrelativetotheothergroupshadhealthinsurancethroughMedicare,andasignificantlylowerproportionwereuninsured(bothp<0.
05)(Table1);privateinsurancewastheprimaryinsurancetypeamongbothAfrican-AmericansandHispanics.
WhilemeantimesincediabetesdiagnosiswasslightlybutsignificantlyhigheramongCaucasians(10.
9years)relativetoAfrican-Americans(9.
4years)andHispanics(9.
4years)(bothp<0.
05),themediansweresimilaracrossethnicities,8years,8years,and9years,respectively.
PainandsensorysymptomsAfrican-AmericanandHispanicpatientswerelesslikelythanCaucasianstoexperiencearangeofsensorysymp-toms(Fig.
1)thatarecharacteristicofneuropathicpainincludingsomesymptomsthatappeartodrivepainseveritysuchassensitivitytotouchandshootingpain.
Thelayeredcross-tabulationsofthesixsymptomsthatweresignificantbyethnicity(electricshock-likepain;painanddiscomfortatnight;stabbingpain;burningpainsensation;shootingpain;sensitivitytotouch)showthatthesedifferencesbyethnicitygenerallyholdforstabbingpain,withasignificanteffectofethnicityfor12ofthe16strata(p<0.
05);shootingpain,whichwassignificantfor11stratap<0.
05);andelectricshockpain(p<0.
05:for9strata)(Table2).
However,significantdifferences(p<0.
05)byethnicitywerelimitedforpainanddiscomfortatnight(only4stratashowedasignificanteffectofethnicity),andburningpainandTable1DemographiccharacteristicsofthepatientpopulationsVariableValueCaucasians(n=823)African-Americans(n=525)Hispanics(n=537)Sex,%Male434842Female575258Age,years,mean55.
7ab41.
037.
0Agedistribution,%18–29years3ab25b2130–39years9ab243840–49years16b202450–59year30ab18b1260–69years30ab10b6≥70years12ab3b1Maritalstatus,%Marriedorlivingasmarried57ab45b72Livingwithdomesticpartner4ab118Single,nevermarried14ab3016Widowed5b4b2Separated2b3b1Divorced18ab7b2Education,%Lessthanhighschool4b67Highschool22b2542aSomecollege—nodegree31b2820aAssociate'sdegree16b159aBachelor'sdegree171819Post-graduatedegree10b82aEmploymentstatus,%Employed38ab6569Retired31ab12b4Disabled19ab10b2Stay-at-homeparent/spouse9ab5b15Unemployed,lookingforwork2ab45Unemployed,notlookingforwork2b24Fulltimestudent<1b12Annualincome,mean$52,300b$53,700b$58,500Insurance,%Medicare44ab16b8Medicaid14b1820Private33ab4752Other6ab32Noinsurance4ab1518ap<0.
05vsAfrican-Americansbp<0.
05vsHispanicsEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page3of9sensitivitytotouch(eachwith6stratathatshowedanethnicityeffect).
Astepwiseregressionanalysiswithaveragepainsever-ityinthepastyearasdependentvariableandthe10painsymptomsasindependentvariablesshowedthatsensi-tivitytotouchisthestrongestpredictorofpain,beingresponsiblefor20%ofthetotalexplainedvarianceinoverallpainscores.
Thesecondstrongestpredictorwasshootingpain(17%),followedbyelectricshock-likepain(10%).
Theoverallmodelwassignificant(p<0.
05),withR2=0.
29andF=59.
077.
WhiletheaveragenumberofreportedpDPNsymptomswasloweramongAfrican-Americans(5.
3)andHispanics(4.
7)relativetoCaucasians(5.
8),thedifferenceswerenotFig.
1TypeofsymptomsTable2Layeredcross-tabulationfortheeffectofethnicityonthepercentofrespondentswhocurrentlyexperiencethepainsymptomsthatweresignificantbyethnicityStratap-valueStabbingpainShootingpainElectricshock-likepainPainanddiscomfortatnightBurningpainSensitivitytotouchControllingforage18–34years<0.
0001<0.
00010.
002NS0.
0010.
00435–54years<0.
0001<0.
0001<0.
0001<0.
001<0.
00010.
001≥55yearsNSNSNSNSNSNSControllingforeducationLessthanhighschool0.
0020.
034NS0.
021NSNSHighschool<0.
0001<0.
00010.
006<0.
0001<0.
0001NSSomecollege–nodegree<0.
00010.
0030.
007NSNS0.
004Associate'sdegreeNS0.
024NSNSNSNSBachelor'sdegreeNSNSNSNSNSNSPost-graduatedegree0.
0090.
031NSNS0.
0240.
007Controllingforincome<$25,0000.
006NSNSNSNSNS$25,000-$34,999<0.
0001<0.
00010.
002NSNS0.
004$35,000-$49,999<0.
0001<0.
00010.
0090.
0050.
006NS$50,000-$74,9990.
0060.
0140.
018NSNSNS$75,000-$99,999NS0.
0010.
013NSNSNS$100,000-$149,9990.
004NS0.
028NS0.
0010.
036≥$150,0000.
007NSNSNSNSNSAbbreviations:NSnotsignificantEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page4of9significant(Fig.
2a).
However,African-AmericansandHispanicswerelesslikelytoratetheirpainasmoderateorsevere,65%and49%,respectively,relativetoCaucasians(87%;bothp<0.
05)(Fig.
2b).
Thisfindingwasconfirmedthroughastepwiselinearregressionwhereethnicity(operationalizedas3dummyvariables,oneeachforCaucasian,African-American,andHispanic)aswellasage,education,andhouseholdincomewereusedasinde-pendentvariablestopredictreportedpainlevels.
TheresultsoftheoverallsignificantmodelshowthatbeingHispanicisthestrongestsignificantpredictoroftheexpe-riencedpainlevels(standardizedbetacoefficientof0.
297),followedbyeducation(betaof0.
211)andbeingAfrican-American(betaof0.
125).
Nootherindependentvariableaddedsignificantexplanatorypower.
PatientandhealthcareproviderdialogueTheproportionofCaucasianswhoreportedreceivingadiagnosisofpDPN(87%)wassignificantlyhigherthanthatofAfrican-Americans(51%)andHispanics(36%)(allp<0.
05)(Fig.
3).
Thissignificancebasedonethnicitywasretainedinlayeredcross-tabulations,with13ofthe16stratashowingsignificance(p≤0.
001;onlypost-graduatedegreeandincomelevelsof$100,000–$149,999and≥$150,000werenotsignificant).
Similarpatternswereobservedwhenstratifiedbypainseverity;consistentlyandsignificantlyhigherproportionsofCaucasiansreportedapDPNdiagnosisrelativetotheothertwopopulationsacrossseveritylevels(allp<0.
05),andHispanicsgenerallyreportedthelowestrateofdiagnosis,althoughthediffer-enceswerenotsignificantvsAfrican-Americans.
SignificantlylowerproportionsofAfrican-AmericanandHispanicpatientsrelativetoCaucasiansreporteddiscussingtheirpainsymptomswiththeirhealthcareprovideracrosspainseveritylevels,(allp<0.
05)(Fig.
4a).
Additionally,amongboththeAfrican-AmericanandHispanicpopulations,therewasconsist-entlylesscomfortwiththeirhealthcareproviders(Fig.
4b),asindicatedbysignificantlylowerproportionsofAfrican-AmericansandHispanicswhoreportedthattheythoughttheirHCPunderstoodtheirculture,aswellasahardertimecommunicating.
Fig.
2PresenceofpDPNsymptoms.
a)Averagenumberofsymptoms.
b)PresenceofmoderateorseverepainFig.
3PatientswhoreceivedadiagnosisofpainfuldiabeticperipheralneuropathyEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page5of9ImpactofpDPNOverallworkimpairmentduetopainwassubstantialamongemployedpatientsinthethreepopulations(Fig.
5).
WhileCaucasiansreportedgreaterworkimpairmentthanAfrican-AmericansandHispanics,noneofthedifferencesbetweengroupswassignificant.
Presenteeismwasatleastthreetimesashighasabsenteeisminallpopulations,andpresenteeismamongCaucasianswassignificantlyhigherrelativetoHispanics,48%and36%,respectively(p<0.
05).
Activityimpairmentwassignificantly(p<0.
05)higheramongCaucasians(56%)relativetoAfrican-Americans(53%)andHispanics(43%)(Fig.
5).
DiscussionThisstudysuggestsnotonlythattherearesignificantdisparitiesacrossculturalgroupsintheirinteractionwithHCPsregardingpDPNanditssymptoms,butthatpresentationofpDPNitselfisalsosignificantlydifferentacrossthesegroups,withlowerpainseverityandfewernumberofpDPNsymptomsreportedamongAfrican-AmericansandHispanicsrelativetoCaucasians.
Inparticular,amongthetypesofsymptoms,onlyforpinsandneedleswasthereconcordanceamongallthreeculturalgroupsforthepercentageofpatientsreportingthissymptom.
Fortheothersymptoms,thepercentofpatientsreportingthesymptomswasgenerallylowestamongHispanicsandhighestamongCaucasians.
Whileithaspreviouslybeenreportedthattherearedifferencesinhowethnicgroupsperceiveandreporttypesandseverityofexperimentalpain[14,15],whichmayinpartresultfromgeneticaswellasculturalfactors[16,17],theobservationsherecontrastwitharecentreviewindicatingthatHispanicsreportgreaterpainsen-sitivityandexperiencegreaterseverityrelativetonon-abFig.
4Interactionbetweenpatientsandtheirhealthcareproviders.
a)Discussionofpain.
b)ComfortlevelofpatientswiththeirhealthcareprovidersEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page6of9HispanicWhites[15].
However,itisalsopossiblethattheseperceptionsmaybedependentonthetypeofpain,i.
e.
,neuropathicornociceptive.
Whetherthesediffer-encesextendtotheclinicalsettinghasnotbeenadequatelyexplored,althoughtheresultsreportedheredosuggestpotentialdifferencesaswellastheneedforfurtherevaluatingpainperceptionsinmulticulturalpop-ulations,includingsensationsrelatedtoneuropathicpainsuchaspDPN.
Therobustnessoftheseresultswasdemonstratedbyadditionalanalysesthatadjustedfordemographicandsocioeconomicfactors,sinceage,educationlevel,andincomemaybepotentialconfoundingfactorsthatcon-tributetopainperceptionsorHCPinteractions.
Theseadditionalanalysessuggestthatregardlessofsocioeco-nomicstatus,ethnicityisageneralfactorinhowsymp-tomsassociatedwithpDPNaremanifestedorperceived.
Additionally,andofpotentialgreaterclinicalrelevance,wasthelargeproportionofAfrican-AmericanandHispanicpopulationswhowere<40yearsofage.
Whileitiswell-recognizedthatdiabetesdisproportionallyaffectsAfrican-AmericansandHispanics[18],toourknowledgethisisthefirststudytosuggestthatthesepopulationsmayalsohaveahighprevalenceofpDPNsymptomsinsuchayoungagegroup,butamorerigorousepidemio-logicstudywouldbeneededtocorroboratetheseobserva-tions.
Theoverallsimilarityacrossethnicitiesfortimesinceadiabetesdiagnosisfurthersuggeststhatdurationofdiabetesisunlikelytomeaningfullyimpacttheobservedresultsandtheirclinicalimplications.
Thedifferencesinsymptomsandseveritywereparal-leledbytheimpactofpainondailyactivitiesontheWPAI:SHPreportedbythethreepopulations;theleastimpairmentwasconsistentlyreportedbyHispanics,andthiswassignificantforActivityimpairmentvsbothotherpopulations,andforPresenteeismvsCaucasians.
ItshouldagainbenotedthattheWPAI:SHPresponsesonworkproductivitywereobtainedonlyfromemployedrespon-dents,whiletheactivityimpairmentquestionwasansweredbyallrespondentsandwaslimitedtoactivitiesotherthanemployment.
TheseobservationsontheWPAI:SHPareconsistentwitharecentreviewsuggestinglowerratesofactivitylimitationamongHispanicswithpainrelativetootherculturalgroupsdespitegreaterpainsensitivity[15].
Amongthoseemployed,presenteeismwasthreetimesthatofabsenteeisminallculturalgroups,suggestingthatthiswastheprimarydriverofworkimpairment,ashasbeenpreviouslyreportedamongpatientswithchronicpainconditions[5].
DespitethepresenceofthesesymptomsandpainofmoderateorsevereseverityinsubstantialproportionsofAfrican-AmericansandHispanics,fewerofthesepatientsreportedreceivingapDPNdiagnosisthanCaucasians.
Thislowerrateofdiagnosismaypotentiallybedue,atleastinpart,totheobservationsrelatedtointeractionsofthesepopulationswiththeirHCPs:FewerAfrican-AmericanandHispanicpatientsreporteddiscussingtheirpainsymptomswiththeirHCP,andtherewasconsistentlylesscomfortwiththeirHCPsinthesegroups.
TheseinteractionswithHCPsareconsistentwiththedisparitiesinhealthcareresourceavailabilityandusethathavebeenreportedamongminoritypopulationsandthatcontributetothechallengeofdiagnosisandmanagementofthesepatients[19].
Inparticular,HispanicshavereportedlanguageandculturalbarrierssuchastheunavailabilityofSpanish-speakinghealthcareprovidersorinterpreters[15,20].
WhiletheselanguageandculturalbarriersmayinpartaccountforthelowercomfortlevelofHispanicswiththeirHCPsinthecurrentstudy,itshouldalsobenotedthatAfrican-Americansreportedasimilarlyhardtimecommunicat-ingwiththeirHCPsasHispanicsdid.
LimitationsAswithanysurveydependentuponrespondents,animportantlimitationispotentialselectionbias,sincepatientswhoagreedtoparticipatemayhavecharacteris-ticsandperceptionsdifferentfromthosewhorefused.
Arelatedlimitationisthatthepatient-leveldataondiagnosis,pain,andsymptomswerebasedonself-report12%48%52%56%14%43%46%53%10%36%39%43%0%10%20%30%40%50%60%AbsenteeismPresenteeismOverallworkimpairmentActivityimpairmentPercentImpairmentCaucasianAfricanAmericanHispanicAmerican****p<0.
05vsHispanicAmericanFig.
5WorklossandproductivityimpairmentassessedusingtheWPAI:SHPEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page7of9and,assuch,maybesubjecttomisunderstandingormis-interpretationofthequestionsthatmayresult,atleastinpart,fromculturaldifferencesacrossthepopulations.
Itshouldalsobenotedthatthisstudydidnotcaptureotherfactorsthatmayhavecontributedtopatients'perceptionsoftheirpainexperience,suchasmood,negativeemotionsandthoughts,poorpaincontrol,orconstruals.
Thesefactors,aswellasothersnotcollected,couldbeapotentialmissingsourceofinformationthatmayhavecontributedtohowsubjectsreportedtheirpainfulsymptomsorinteractionswiththeirHCPs,andwarrantfurtherevaluationinfuturestudies.
Whileuseofbothinternetandphoneassurveymodalitiescouldbecriticized,suchadesignwasneces-sarytoreachthetargetpopulations,andtheinabilitytodisentangletheadministrationmodalityfromtheresultsacrossthepopulationsrepresentsanotherlimitation.
Lastly,thesurveyresultsreflectanunweightedsample,andthusmaynotnecessarilybereflectiveorrepresenta-tiveoftheentiregeneralpopulationintheUnitedStates.
However,thefindingsprovidedirectionalinsightsthatcanbeusedtooptimizepatientcare.
ConclusionsSignificantdifferencesinpatientexperiencesofpDPNsymptomsandpainseveritywerereportedacrosscul-turalgroupsincludingAfrican-Americans,Hispanics,andCaucasians;African-AmericansandHispanicswerelesslikelytoexperiencethesamesensationsasCauca-sianpatientsandreportedlowerpainratings.
Furtherevaluationisneededtodeterminewhatmayaccountfortheseobserveddifferences.
DifferentialratesofpDPNdiagnosisandcomfortlevelswithHCPswerealsoreportedinthismulticulturalpopulation,withthediffer-encesprovidingsupportforbarriersthatcontributetodisparitiesinhealthcareamongspecificpopulations.
TheseresultssuggestaneedtobroadenpDPNeduca-tionalinitiativesamongbothpatientsandclinicians.
Whilepatientintiativesshouldespeciallytargetmulticul-turalpopulations,thegoalsofclinicianinitiativesshouldbetoincreaseattentionthatsymptomsmaydifferamongindividualswithdifferentculturalbackgroundsandtoimprovepatient-HCPdialoguebyencouragingdiscussionofpDPNsymptomsandtheirimpactinmulticulturalsettings.
AdditionalfileAdditionalfile1:MulticulturalpDPNResearchPatientSurvey.
(DOCX260kb)AbbreviationsBPI:BriefPainInventory;HCP:Healthcareprovider;pDPN:Painfuldiabeticperipheralneuropathy;WPAI:SHP:WorkProductivityandAssessmentQuestionnairedisease-specificversionAcknowledgementsEditorial/medicalwritingsupportwasprovidedbyE.
JayBienenandwasfundedbyPfizer.
FundingThisstudywasconductedbyKeltonGlobalandsponsoredbyPfizerInc.
AvailabilityofdataandmaterialsThesurveyisavailableasElectronicSupplementaryMaterialOnlineResource1.
Dataareavailableonrequestfromthecorrespondingauthor.
Authors'contributionsAllauthorsmettheInternationalCommitteeofMedicalJournalEditors(ICMJE)recommendationsforauthorship.
AS,AHA,JCC,PT,BPandMMTwereinvolvedinconceptionanddesignofthestudyincludingdevelopmentofthesurveyinstrument.
MEcarriedoutdataacquisition.
MEandJCCanalyzedandinterpretedthedatawithfurtherinputfromtheremainingauthors.
Allauthorswereinvolvedindraftingthearticleandrevisingitcriticallyforimportantintellectualcontent.
Allauthorsapprovedthefinalversiontobesubmittedforpublication.
EthicsapprovalandconsenttoparticipateEthics/InstitutionalReviewBoard(IRB)approvalwasnotobtainedforthisstudy,whichwasconductedbyKeltonGlobal,amarketresearchfirm,whoaccessedexistingparticipantpanelsacrosstheUS.
;allsubjectshadpreviouslyagreedtoparticipateinthenationalresearchpanelthatwasaccessed.
Additionally,allsubjectswereadvised,eitherverballyforphoneparticipation,orviaaninitialonlinescreenforInternetparticipationthat"Theresultsmayappearinleadingmediaoutletsinthecomingweeks,butyouranswerswillremainconfidentialandanonymous.
"ConsentforpublicationNotapplicableCompetinginterestsMEisanemployeeofKeltonGlobal.
AHAwasanemployeeandshareholderofPfizeratthetimeofthestudyanddevelopmentofthemanuscript.
BP,JCC,PH,andASarepaidemployeesandshareholdersofPfizer.
MMTisapracticingneurologistandreportsnoconflictsofinterest.
Publisher'sNoteSpringerNatureremainsneutralwithregardtojurisdictionalclaimsinpublishedmapsandinstitutionalaffiliations.
Authordetails1KeltonCommunications,CulverCity,CA,USA.
2PfizerInc.
,235East42ndStreet,NewYork,NY10017,USA.
3PfizerInc.
,Groton,CT,USA.
4PalmBeachNeurologicalCenter,PalmBeachGardens,FL,USA.
Received:23August2017Accepted:6December2017References1.
SadoskyA,McDermottAM,BrandenburgNA,StraussM.
Areviewoftheepidemiologyofpainfuldiabeticperipheralneuropathy,post-herpeticneuralgia,andlesscommonlystudiedneuropathicpainconditions.
PainPract.
2008;8(1):45–56.
2.
JambartS,AmmacheZ,HaddadF,YounesA,HassounA,AbdallaK,SelwanCA,SunnaN,WajsbrotD,YouseifE.
PrevalenceofpainfuldiabeticperipheralneuropathyamongpatientswithdiabetesmellitusintheMiddleEastregion.
JIntMedRes.
2011;39(2):366–77.
3.
AllemanCJ,WesterhoutKY,HensenM,ChambersC,StokerM,LongS,vanNootenFE.
HumanisticandeconomicburdenofpainfuldiabeticperipheralneuropathyinEurope:areviewoftheliterature.
DiabetesResClinPract.
2015;109(2):215–25.
4.
vanHeckeO,AustinSK,KhanRA,SmithBH,TorranceN.
Neuropathicpaininthegeneralpopulation:asystematicreviewofepidemiologicalstudies.
Pain.
2014;155(4):654–62.
5.
StewartWF,RicciJA,CheeE,HirschAG,BrandenburgN.
LostproductivetimeandcostsduetodiabetesanddiabeticneuropathicpainintheUSworkforce.
JOccupEnvironMed.
2007;49(6):672–9.
Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page8of96.
daCostaDiBonaventuraM,CappelleriJC,JoshiAV.
Alongitudinalassessmentofpainfuldiabeticperipheralneuropathyonhealthstatus,productivity,andhealthcareutilizationandcost.
PainMed.
2011;12(1):118–26.
7.
SadoskyA,MardekianJ,ParsonsB,HoppsM,BienenEJ,MarkmanJ.
Healthcareutilizationandcostsindiabetesrelativetotheclinicalspectrumofpainfuldiabeticperipheralneuropathy.
JDiabetesComplicat.
2015;29(2):212–7.
8.
SadoskyA,HopperJ,ParsonsB.
Painfuldiabeticperipheralneuropathy:resultsofasurveycharacterizingtheperspectivesandmisperceptionsofpatientsandhealthcarepractitioners.
Patient.
2014;7(1):107–14.
9.
PortenoyR.
Developmentandtestingofaneuropathicpainscreeningquestionnaire:IDpain.
CurrMedResOpin.
2006;22(8):1555–65.
10.
CleelandCS,RyanKM.
Painassessment:globaluseofthebriefpaininventory.
AnnAcadMedSingap.
1994;23(2):129–38.
11.
WorkProductivityandActivityImpairmentQuestionnaire:SpecificHealthProblemV2.
0(WPAI:SHP)[http://www.
reillyassociates.
net/WPAI_SHP.
html].
12.
ZelmanD,DukesE,BrandenburgN,BostromA,GoreM.
Identificationofcut-pointsformild,moderateandseverepainduetodiabeticperipheralneuropathy.
Pain.
2005;115(2):29–36.
13.
KleinbaumDG,KupperLL,NizamA,RosenbergES.
Appliedregressionanalysisandothermultivariatemethods.
5thed.
Boston:CengageLearning;2014.
14.
Rahim-WilliamsB,RileyJL3rd,WilliamsAK,FillingimRB.
Aquantitativereviewofethnicgroupdifferencesinexperimentalpainresponse:dobiology,psychology,andculturematterPainMed.
2012;13(4):522–40.
15.
HollingsheadNA,Ashburn-NardoL,StewartJC,HirshAT.
ThepainexperienceofHispanicAmericans:acriticalliteraturereviewandconceptualmodel.
JPain.
2016;17(5):513–28.
16.
KimH,NeubertJK,SanMiguelA,XuK,KrishnarajuRK,IadarolaMJ,GoldmanD,DionneRA.
Geneticinfluenceonvariabilityinhumanacuteexperimentalpainsensitivityassociatedwithgender,ethnicityandpsychologicaltemperament.
Pain.
2004;109(3):488–96.
17.
CampbellCM,EdwardsRR.
Ethnicdifferencesinpainandpainmanagement.
PainManag.
2012;2(3):219–30.
18.
NationalDiabetesStatisticsReport:EstimatesofDiabetesandItsBurdenintheUnitedStates,2014.
Atlanta:U.
S.
DepartmentofHealthandHumanServices.
http://www.
thefdha.
org/pdf/diabetes.
pdf.
19.
NationalHealthcareDisparitiesReport,2013.
Publication#14–0006[http://www.
ahrq.
gov/research/findings/nhqrdr/nhdr13/2013nhdr.
pdf].
20.
BetancourtJR,CorbettJ,BondarykMR.
Addressingdisparitiesandachievingequity:culturalcompetence,ethics,andhealth-caretransformation.
Chest.
2014;145(1):143–8.
Weacceptpre-submissioninquiriesOurselectortoolhelpsyoutondthemostrelevantjournalWeprovideroundtheclockcustomersupportConvenientonlinesubmissionThoroughpeerreviewInclusioninPubMedandallmajorindexingservicesMaximumvisibilityforyourresearchSubmityourmanuscriptatwww.
biomedcentral.
com/submitSubmityournextmanuscripttoBioMedCentralandwewillhelpyouateverystep:Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page9of9
Alexander2,JosephC.
Cappelleri3,PatrickHlavacek2,BruceParsons2,AlesiaSadosky2*andMichaelM.
Tuchman4AbstractBackground:Sincefewstudieshavecharacterizedpainfuldiabeticperipheralneuropathy(pDPN)symptomsinmulticulturalpopulations,thisstudyfieldedasurveytobetterunderstandpDPNanditsimpactinAfrican-American,Caucasian,andHispanicpopulations.
Methods:KeltonfieldedasurveybyphoneorInternet,inEnglishorSpanish,amongadultswithpDPNsymptomsintheUnitedStatesbetweenAugustandOctober2015;African-AmericansandHispanicswereoversampledtoachieveatleast500subjectsforeachgroup.
PatientswererequiredtohavebeendiagnosedwithpDPNorscore≥3onIDPainvalidatedscreeningtool.
ThesurveyelicitedinformationonpDPNsymptomsandinteractionswithhealthcareproviders(HCPs),andincludedtheBriefPainInventoryandpain-specificWorkProductivityandAssessmentQuestionnaire(WPAI:SHP).
Results:Respondentsincluded823Caucasians,525African-Americans,and537Hispanics;approximatelyhalfofAfrican-AmericansandHispanicswere<40yearsofage,vs12%ofCaucasians.
PainwaslesslikelytoberatedmoderateorseverebyAfrican-Americans(65%)andHispanics(49%)relativetoCaucasians(87%;p<0.
05).
African-AmericansandHispanicswerelesslikelythanCaucasianstoreportexperiencingspecificpDPNsensorysymptoms.
SignificantlyfewerAfrican-AmericansandHispanicsreportedreceivingapDPNdiagnosisrelativetoCaucasians(p<0.
05),andhigherproportionsofAfrican-AmericansandHispanicsreporteddifficultycommunicatingwiththeirHCP(p<0.
05).
WPAI:SHPactivityimpairmentwaslowerinHispanics(43%)relativetoAfrican-Americans(53%)andCaucasian(56%;p<0.
05).
Conclusions:MulticulturalpatientsreporteddifferencesinpDPNsymptomsandpainrelativetoCaucasians,andfewerreceivedapDPNdiagnosis.
Whilefurtherevaluationisneededtounderstandthesedifferences,thesedatasuggestaneedtobroadenpDPNeducationalinitiativestoimprovepatient-HCPdialogueandencouragediscussionofpDPNsymptomsandtheirimpactinamulticulturalsetting.
Keywords:Painfuldiabeticperipheralneuropathy,Race,Ethnicity,Pain,Productivity*Correspondence:Alesia.
sadosky@pfizer.
com2PfizerInc.
,235East42ndStreet,NewYork,NY10017,USAFulllistofauthorinformationisavailableattheendofthearticleTheAuthor(s).
2017OpenAccessThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12DOI10.
1186/s40842-017-0051-2BackgroundDiabeticperipheralneuropathy(DPN)isacommoncomplicationofType1andType2diabetesthatischaracterizedbynervedamage.
WhenDPNpresentswithpainfulsymptomstheconditionisknownaspainfuldiabeticperipheralneuropathy(pDPN).
Whiletheepi-demiologyofpDPNhasnotbeenwell-characterized,anoverallprevalenceof15%hasbeenestimatedinthedia-beticpopulation[1].
However,prevalenceratesexceed-ing30%inpatientswithdiabeteshavebeenreportedinmorerecentregionalstudies[2,3],andasystematicreviewofneuropathicpaininthegeneralpopulationreportedapDPNprevalenceof0.
8%thatrepresentsapproximately26%ofindividualswithType2diabetes[4].
Thesubstantialpatientandeconomicburdensassoci-atedwithpDPNarewell-recognizedandincludereduc-tionsinpatientfunction,qualityoflife,andproductivity[5,6],aswellasgreaterhealthcareresourceutilizationandcostsrelativetopatientswithdiabetesandwithDPNwithoutpain[7].
Despitestudiesevaluatingqualityoflifeandotherpatient-reportedoutcomesinpDPN,therearelimiteddataontheseverityandimpactofpainfulpDPNsymp-tomsfromthepatient'sperspective.
Asurveyinpatientsandclinicianswhotreatpatientswithdiabetesnotonlyshowedthatmisperceptionsonthecauseandmanage-mentofpDPNwerecommoninbothstakeholdergroupsbutalsoindicatedadditionaldisparitiesbetweenpatientandclinicianperspectivesregardingcommunica-tion,severity,andtreatment[8].
However,lessisknownaboutthepatientperceptionsofpDPNandinteractionsbetweenthesepatientsandtheirhealthcareproviders(HCPs)inamulticulturalpopulation.
Therefore,theobjectiveofthisstudywastocharacterizetheimpactofpDPNandidentifybarrierstoitsmanagementinamulticulturalUSpopulationwithafocusonAfrican-AmericansandHispanicsrelativetoCaucasians.
MethodsDesignandpopulationsKeltonfieldedasurveyamongpDPNpatientsintheUnitedStatesbetweenAugustandOctober2015.
Forinclusion,patientswererequiredtobeadults(≥18yearsold)whoself-reportedbeingdiagnosedwitheitherType1orType2diabetesandeitherself-reportedhavingreceivedadiagnosisofpDPNbyanHCPorhadascore≥3onIDPain[9](i.
e.
,experienced≥3ofthefollowingsymptomswithinthepastweek:pinsandneedles,hot/burning,numbness,electricalshocks,orpainthatismadeworsewiththetouchofclothingorbedsheets).
IDPainisavalidatedmeasurethatisusedtoscreenpatientsforthepresenceofneuropathicpainbasedonitsdemonstratedabilitytodiscriminatebetweennociceptiveandneuropathicpain[9].
Thesurvey,whichwasdevelopedwithoutpatientinputbutincollaborationwithexpertsinthefield,includingclinicians,wasadministeredbyInternetamongCaucasians,andbyeitherInternetorphoneamongAfrican-AmericansandHispanics,withInternetrespondentsrecruitedfromanationalresearchpanelandphonerespondentsrecruitedfrompurchasedphonelists.
Oversamplingviaphonewasperformedtoachieveagoalofatleast500Hispanicpatientsand500African-Americanpatients.
ThesurveycouldbecompletedinEnglishorSpanish,withtheSpanishversionback-translatedbynativeSpanish-speakerstoensureaccuracyofthequestionnaire.
Thesurvey(Additionalfile1)consistedofbatteriesofquestionsthatwereinpartderivedfromaprevious,simi-larsurvey[8].
ThegoalwastocaptureperspectivesonpDPNsymptoms(numbness;pinsandneedles;painordiscomfortatnight;tinglingorpricklingsensation;sensi-tivitytotouch;burningpainorsensation;shootingpain;radiatingpain;stinging;stabbingpain;electricshock-likesymptomsorsuddenpainattacks;throbbingpain),perceptionsofpainassociatedwiththesymptoms,andhowpatientsdiscussthesesymptomswiththeirphysician.
Additionally,thesurveyincludedtheBriefPainInven-tory(BPI)[10]andtheWorkProductivityandAssessmentQuestionnairedisease-specificversion(WPAI:SHP)adaptedforpain[11],bothofwhichdemonstratesoundpsychometricmeasurementpropertiesandhavebeenusedasoutcomesacrossawidevarietyofdiseasestates.
TheBPIratesworst,least,andaveragepaininthepast24handtheaveragepainsubscalewasusedtocategorizepainasmild,moderate,andseverebasedonestablishedcutpointsfortheaveragepainscaleof0–3formild,4–6formoderate,and7–10forsevere[12].
TheWPAI:SHPmeasuresimpactofthediseaseonproductivityatworkduetoabsenteeism(worktimemissed),presenteeism(impairmentwhileatwork),overallworkimpairment,andactivityimpairmentoutsideofworkduringthepast7days.
StatisticalanalysisSurveyresultsreflectanunweightedsample.
Themarginoferrorwas±3.
1%forthetotalpatientsampleand4.
0%fortheoversampledgroups.
Analysesforcategoricaldataandcontinuousdatawereconductedusingchi-squaretestsandt-tests,respectively.
Theimpactofethnicitywasexploredbasedonthecombinedmainsampleandover-sampleandcontrolledforeffectsofage,education,andhouseholdincomeusinglayeredcross-tabulations(chi-squaretests)andstepwiselinearregression[13].
Thecross-tabulationswereconductedusing16demographicstrata:3agegroups(18–34years,35–54years,and≥55years),6educationlevels,and7incomelevelsshowninthedemographicstable(Table1).
Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page2of9Stepwiselinearregressionwasalsoperformedamongthemainsample,usingpainseverityasthedependentvariableand10itemsrelatedtothepatients'experiencewithsymptomsasindependentvariables(numbness;pinsandneedles;painordiscomfortatnight;tinglingorpricklingsensation;sensitivitytotouch;burningpainorsensation;shootingpain;stinging;stabbingpain;electricshock-likesymptomsorsuddenpainattacks).
AllanalyseswereperformedusingIBMSPSSStatistics23.
ResultsRespondentpopulationsTable1presentsthedemographiccharacteristicsofthemulticulturalpopulations,andshowsthatmeanagewassignificantlyhigher(p<0.
05)amongCaucasiansthanAfrican-AmericansandHispanics,anddifferenceswerealsoobservedintheagedistribution.
AlmosthalfoftheAfrican-Americans(49%)andmorethanhalfoftheHis-panics(59%)wereunder40yearsofage,comparedwithonly12%ofCaucasians.
Caucasianshadthelowestrateofemploymentandthehighestrateofretireesamongthethreeculturalgroups,andannualincomewashigh-estinHispanics,lowestamongCaucasians.
Consistentwiththeolderdemographic,asignificantlygreaterpro-portionofCaucasiansrelativetotheothergroupshadhealthinsurancethroughMedicare,andasignificantlylowerproportionwereuninsured(bothp<0.
05)(Table1);privateinsurancewastheprimaryinsurancetypeamongbothAfrican-AmericansandHispanics.
WhilemeantimesincediabetesdiagnosiswasslightlybutsignificantlyhigheramongCaucasians(10.
9years)relativetoAfrican-Americans(9.
4years)andHispanics(9.
4years)(bothp<0.
05),themediansweresimilaracrossethnicities,8years,8years,and9years,respectively.
PainandsensorysymptomsAfrican-AmericanandHispanicpatientswerelesslikelythanCaucasianstoexperiencearangeofsensorysymp-toms(Fig.
1)thatarecharacteristicofneuropathicpainincludingsomesymptomsthatappeartodrivepainseveritysuchassensitivitytotouchandshootingpain.
Thelayeredcross-tabulationsofthesixsymptomsthatweresignificantbyethnicity(electricshock-likepain;painanddiscomfortatnight;stabbingpain;burningpainsensation;shootingpain;sensitivitytotouch)showthatthesedifferencesbyethnicitygenerallyholdforstabbingpain,withasignificanteffectofethnicityfor12ofthe16strata(p<0.
05);shootingpain,whichwassignificantfor11stratap<0.
05);andelectricshockpain(p<0.
05:for9strata)(Table2).
However,significantdifferences(p<0.
05)byethnicitywerelimitedforpainanddiscomfortatnight(only4stratashowedasignificanteffectofethnicity),andburningpainandTable1DemographiccharacteristicsofthepatientpopulationsVariableValueCaucasians(n=823)African-Americans(n=525)Hispanics(n=537)Sex,%Male434842Female575258Age,years,mean55.
7ab41.
037.
0Agedistribution,%18–29years3ab25b2130–39years9ab243840–49years16b202450–59year30ab18b1260–69years30ab10b6≥70years12ab3b1Maritalstatus,%Marriedorlivingasmarried57ab45b72Livingwithdomesticpartner4ab118Single,nevermarried14ab3016Widowed5b4b2Separated2b3b1Divorced18ab7b2Education,%Lessthanhighschool4b67Highschool22b2542aSomecollege—nodegree31b2820aAssociate'sdegree16b159aBachelor'sdegree171819Post-graduatedegree10b82aEmploymentstatus,%Employed38ab6569Retired31ab12b4Disabled19ab10b2Stay-at-homeparent/spouse9ab5b15Unemployed,lookingforwork2ab45Unemployed,notlookingforwork2b24Fulltimestudent<1b12Annualincome,mean$52,300b$53,700b$58,500Insurance,%Medicare44ab16b8Medicaid14b1820Private33ab4752Other6ab32Noinsurance4ab1518ap<0.
05vsAfrican-Americansbp<0.
05vsHispanicsEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page3of9sensitivitytotouch(eachwith6stratathatshowedanethnicityeffect).
Astepwiseregressionanalysiswithaveragepainsever-ityinthepastyearasdependentvariableandthe10painsymptomsasindependentvariablesshowedthatsensi-tivitytotouchisthestrongestpredictorofpain,beingresponsiblefor20%ofthetotalexplainedvarianceinoverallpainscores.
Thesecondstrongestpredictorwasshootingpain(17%),followedbyelectricshock-likepain(10%).
Theoverallmodelwassignificant(p<0.
05),withR2=0.
29andF=59.
077.
WhiletheaveragenumberofreportedpDPNsymptomswasloweramongAfrican-Americans(5.
3)andHispanics(4.
7)relativetoCaucasians(5.
8),thedifferenceswerenotFig.
1TypeofsymptomsTable2Layeredcross-tabulationfortheeffectofethnicityonthepercentofrespondentswhocurrentlyexperiencethepainsymptomsthatweresignificantbyethnicityStratap-valueStabbingpainShootingpainElectricshock-likepainPainanddiscomfortatnightBurningpainSensitivitytotouchControllingforage18–34years<0.
0001<0.
00010.
002NS0.
0010.
00435–54years<0.
0001<0.
0001<0.
0001<0.
001<0.
00010.
001≥55yearsNSNSNSNSNSNSControllingforeducationLessthanhighschool0.
0020.
034NS0.
021NSNSHighschool<0.
0001<0.
00010.
006<0.
0001<0.
0001NSSomecollege–nodegree<0.
00010.
0030.
007NSNS0.
004Associate'sdegreeNS0.
024NSNSNSNSBachelor'sdegreeNSNSNSNSNSNSPost-graduatedegree0.
0090.
031NSNS0.
0240.
007Controllingforincome<$25,0000.
006NSNSNSNSNS$25,000-$34,999<0.
0001<0.
00010.
002NSNS0.
004$35,000-$49,999<0.
0001<0.
00010.
0090.
0050.
006NS$50,000-$74,9990.
0060.
0140.
018NSNSNS$75,000-$99,999NS0.
0010.
013NSNSNS$100,000-$149,9990.
004NS0.
028NS0.
0010.
036≥$150,0000.
007NSNSNSNSNSAbbreviations:NSnotsignificantEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page4of9significant(Fig.
2a).
However,African-AmericansandHispanicswerelesslikelytoratetheirpainasmoderateorsevere,65%and49%,respectively,relativetoCaucasians(87%;bothp<0.
05)(Fig.
2b).
Thisfindingwasconfirmedthroughastepwiselinearregressionwhereethnicity(operationalizedas3dummyvariables,oneeachforCaucasian,African-American,andHispanic)aswellasage,education,andhouseholdincomewereusedasinde-pendentvariablestopredictreportedpainlevels.
TheresultsoftheoverallsignificantmodelshowthatbeingHispanicisthestrongestsignificantpredictoroftheexpe-riencedpainlevels(standardizedbetacoefficientof0.
297),followedbyeducation(betaof0.
211)andbeingAfrican-American(betaof0.
125).
Nootherindependentvariableaddedsignificantexplanatorypower.
PatientandhealthcareproviderdialogueTheproportionofCaucasianswhoreportedreceivingadiagnosisofpDPN(87%)wassignificantlyhigherthanthatofAfrican-Americans(51%)andHispanics(36%)(allp<0.
05)(Fig.
3).
Thissignificancebasedonethnicitywasretainedinlayeredcross-tabulations,with13ofthe16stratashowingsignificance(p≤0.
001;onlypost-graduatedegreeandincomelevelsof$100,000–$149,999and≥$150,000werenotsignificant).
Similarpatternswereobservedwhenstratifiedbypainseverity;consistentlyandsignificantlyhigherproportionsofCaucasiansreportedapDPNdiagnosisrelativetotheothertwopopulationsacrossseveritylevels(allp<0.
05),andHispanicsgenerallyreportedthelowestrateofdiagnosis,althoughthediffer-enceswerenotsignificantvsAfrican-Americans.
SignificantlylowerproportionsofAfrican-AmericanandHispanicpatientsrelativetoCaucasiansreporteddiscussingtheirpainsymptomswiththeirhealthcareprovideracrosspainseveritylevels,(allp<0.
05)(Fig.
4a).
Additionally,amongboththeAfrican-AmericanandHispanicpopulations,therewasconsist-entlylesscomfortwiththeirhealthcareproviders(Fig.
4b),asindicatedbysignificantlylowerproportionsofAfrican-AmericansandHispanicswhoreportedthattheythoughttheirHCPunderstoodtheirculture,aswellasahardertimecommunicating.
Fig.
2PresenceofpDPNsymptoms.
a)Averagenumberofsymptoms.
b)PresenceofmoderateorseverepainFig.
3PatientswhoreceivedadiagnosisofpainfuldiabeticperipheralneuropathyEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page5of9ImpactofpDPNOverallworkimpairmentduetopainwassubstantialamongemployedpatientsinthethreepopulations(Fig.
5).
WhileCaucasiansreportedgreaterworkimpairmentthanAfrican-AmericansandHispanics,noneofthedifferencesbetweengroupswassignificant.
Presenteeismwasatleastthreetimesashighasabsenteeisminallpopulations,andpresenteeismamongCaucasianswassignificantlyhigherrelativetoHispanics,48%and36%,respectively(p<0.
05).
Activityimpairmentwassignificantly(p<0.
05)higheramongCaucasians(56%)relativetoAfrican-Americans(53%)andHispanics(43%)(Fig.
5).
DiscussionThisstudysuggestsnotonlythattherearesignificantdisparitiesacrossculturalgroupsintheirinteractionwithHCPsregardingpDPNanditssymptoms,butthatpresentationofpDPNitselfisalsosignificantlydifferentacrossthesegroups,withlowerpainseverityandfewernumberofpDPNsymptomsreportedamongAfrican-AmericansandHispanicsrelativetoCaucasians.
Inparticular,amongthetypesofsymptoms,onlyforpinsandneedleswasthereconcordanceamongallthreeculturalgroupsforthepercentageofpatientsreportingthissymptom.
Fortheothersymptoms,thepercentofpatientsreportingthesymptomswasgenerallylowestamongHispanicsandhighestamongCaucasians.
Whileithaspreviouslybeenreportedthattherearedifferencesinhowethnicgroupsperceiveandreporttypesandseverityofexperimentalpain[14,15],whichmayinpartresultfromgeneticaswellasculturalfactors[16,17],theobservationsherecontrastwitharecentreviewindicatingthatHispanicsreportgreaterpainsen-sitivityandexperiencegreaterseverityrelativetonon-abFig.
4Interactionbetweenpatientsandtheirhealthcareproviders.
a)Discussionofpain.
b)ComfortlevelofpatientswiththeirhealthcareprovidersEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page6of9HispanicWhites[15].
However,itisalsopossiblethattheseperceptionsmaybedependentonthetypeofpain,i.
e.
,neuropathicornociceptive.
Whetherthesediffer-encesextendtotheclinicalsettinghasnotbeenadequatelyexplored,althoughtheresultsreportedheredosuggestpotentialdifferencesaswellastheneedforfurtherevaluatingpainperceptionsinmulticulturalpop-ulations,includingsensationsrelatedtoneuropathicpainsuchaspDPN.
Therobustnessoftheseresultswasdemonstratedbyadditionalanalysesthatadjustedfordemographicandsocioeconomicfactors,sinceage,educationlevel,andincomemaybepotentialconfoundingfactorsthatcon-tributetopainperceptionsorHCPinteractions.
Theseadditionalanalysessuggestthatregardlessofsocioeco-nomicstatus,ethnicityisageneralfactorinhowsymp-tomsassociatedwithpDPNaremanifestedorperceived.
Additionally,andofpotentialgreaterclinicalrelevance,wasthelargeproportionofAfrican-AmericanandHispanicpopulationswhowere<40yearsofage.
Whileitiswell-recognizedthatdiabetesdisproportionallyaffectsAfrican-AmericansandHispanics[18],toourknowledgethisisthefirststudytosuggestthatthesepopulationsmayalsohaveahighprevalenceofpDPNsymptomsinsuchayoungagegroup,butamorerigorousepidemio-logicstudywouldbeneededtocorroboratetheseobserva-tions.
Theoverallsimilarityacrossethnicitiesfortimesinceadiabetesdiagnosisfurthersuggeststhatdurationofdiabetesisunlikelytomeaningfullyimpacttheobservedresultsandtheirclinicalimplications.
Thedifferencesinsymptomsandseveritywereparal-leledbytheimpactofpainondailyactivitiesontheWPAI:SHPreportedbythethreepopulations;theleastimpairmentwasconsistentlyreportedbyHispanics,andthiswassignificantforActivityimpairmentvsbothotherpopulations,andforPresenteeismvsCaucasians.
ItshouldagainbenotedthattheWPAI:SHPresponsesonworkproductivitywereobtainedonlyfromemployedrespon-dents,whiletheactivityimpairmentquestionwasansweredbyallrespondentsandwaslimitedtoactivitiesotherthanemployment.
TheseobservationsontheWPAI:SHPareconsistentwitharecentreviewsuggestinglowerratesofactivitylimitationamongHispanicswithpainrelativetootherculturalgroupsdespitegreaterpainsensitivity[15].
Amongthoseemployed,presenteeismwasthreetimesthatofabsenteeisminallculturalgroups,suggestingthatthiswastheprimarydriverofworkimpairment,ashasbeenpreviouslyreportedamongpatientswithchronicpainconditions[5].
DespitethepresenceofthesesymptomsandpainofmoderateorsevereseverityinsubstantialproportionsofAfrican-AmericansandHispanics,fewerofthesepatientsreportedreceivingapDPNdiagnosisthanCaucasians.
Thislowerrateofdiagnosismaypotentiallybedue,atleastinpart,totheobservationsrelatedtointeractionsofthesepopulationswiththeirHCPs:FewerAfrican-AmericanandHispanicpatientsreporteddiscussingtheirpainsymptomswiththeirHCP,andtherewasconsistentlylesscomfortwiththeirHCPsinthesegroups.
TheseinteractionswithHCPsareconsistentwiththedisparitiesinhealthcareresourceavailabilityandusethathavebeenreportedamongminoritypopulationsandthatcontributetothechallengeofdiagnosisandmanagementofthesepatients[19].
Inparticular,HispanicshavereportedlanguageandculturalbarrierssuchastheunavailabilityofSpanish-speakinghealthcareprovidersorinterpreters[15,20].
WhiletheselanguageandculturalbarriersmayinpartaccountforthelowercomfortlevelofHispanicswiththeirHCPsinthecurrentstudy,itshouldalsobenotedthatAfrican-Americansreportedasimilarlyhardtimecommunicat-ingwiththeirHCPsasHispanicsdid.
LimitationsAswithanysurveydependentuponrespondents,animportantlimitationispotentialselectionbias,sincepatientswhoagreedtoparticipatemayhavecharacteris-ticsandperceptionsdifferentfromthosewhorefused.
Arelatedlimitationisthatthepatient-leveldataondiagnosis,pain,andsymptomswerebasedonself-report12%48%52%56%14%43%46%53%10%36%39%43%0%10%20%30%40%50%60%AbsenteeismPresenteeismOverallworkimpairmentActivityimpairmentPercentImpairmentCaucasianAfricanAmericanHispanicAmerican****p<0.
05vsHispanicAmericanFig.
5WorklossandproductivityimpairmentassessedusingtheWPAI:SHPEichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page7of9and,assuch,maybesubjecttomisunderstandingormis-interpretationofthequestionsthatmayresult,atleastinpart,fromculturaldifferencesacrossthepopulations.
Itshouldalsobenotedthatthisstudydidnotcaptureotherfactorsthatmayhavecontributedtopatients'perceptionsoftheirpainexperience,suchasmood,negativeemotionsandthoughts,poorpaincontrol,orconstruals.
Thesefactors,aswellasothersnotcollected,couldbeapotentialmissingsourceofinformationthatmayhavecontributedtohowsubjectsreportedtheirpainfulsymptomsorinteractionswiththeirHCPs,andwarrantfurtherevaluationinfuturestudies.
Whileuseofbothinternetandphoneassurveymodalitiescouldbecriticized,suchadesignwasneces-sarytoreachthetargetpopulations,andtheinabilitytodisentangletheadministrationmodalityfromtheresultsacrossthepopulationsrepresentsanotherlimitation.
Lastly,thesurveyresultsreflectanunweightedsample,andthusmaynotnecessarilybereflectiveorrepresenta-tiveoftheentiregeneralpopulationintheUnitedStates.
However,thefindingsprovidedirectionalinsightsthatcanbeusedtooptimizepatientcare.
ConclusionsSignificantdifferencesinpatientexperiencesofpDPNsymptomsandpainseveritywerereportedacrosscul-turalgroupsincludingAfrican-Americans,Hispanics,andCaucasians;African-AmericansandHispanicswerelesslikelytoexperiencethesamesensationsasCauca-sianpatientsandreportedlowerpainratings.
Furtherevaluationisneededtodeterminewhatmayaccountfortheseobserveddifferences.
DifferentialratesofpDPNdiagnosisandcomfortlevelswithHCPswerealsoreportedinthismulticulturalpopulation,withthediffer-encesprovidingsupportforbarriersthatcontributetodisparitiesinhealthcareamongspecificpopulations.
TheseresultssuggestaneedtobroadenpDPNeduca-tionalinitiativesamongbothpatientsandclinicians.
Whilepatientintiativesshouldespeciallytargetmulticul-turalpopulations,thegoalsofclinicianinitiativesshouldbetoincreaseattentionthatsymptomsmaydifferamongindividualswithdifferentculturalbackgroundsandtoimprovepatient-HCPdialoguebyencouragingdiscussionofpDPNsymptomsandtheirimpactinmulticulturalsettings.
AdditionalfileAdditionalfile1:MulticulturalpDPNResearchPatientSurvey.
(DOCX260kb)AbbreviationsBPI:BriefPainInventory;HCP:Healthcareprovider;pDPN:Painfuldiabeticperipheralneuropathy;WPAI:SHP:WorkProductivityandAssessmentQuestionnairedisease-specificversionAcknowledgementsEditorial/medicalwritingsupportwasprovidedbyE.
JayBienenandwasfundedbyPfizer.
FundingThisstudywasconductedbyKeltonGlobalandsponsoredbyPfizerInc.
AvailabilityofdataandmaterialsThesurveyisavailableasElectronicSupplementaryMaterialOnlineResource1.
Dataareavailableonrequestfromthecorrespondingauthor.
Authors'contributionsAllauthorsmettheInternationalCommitteeofMedicalJournalEditors(ICMJE)recommendationsforauthorship.
AS,AHA,JCC,PT,BPandMMTwereinvolvedinconceptionanddesignofthestudyincludingdevelopmentofthesurveyinstrument.
MEcarriedoutdataacquisition.
MEandJCCanalyzedandinterpretedthedatawithfurtherinputfromtheremainingauthors.
Allauthorswereinvolvedindraftingthearticleandrevisingitcriticallyforimportantintellectualcontent.
Allauthorsapprovedthefinalversiontobesubmittedforpublication.
EthicsapprovalandconsenttoparticipateEthics/InstitutionalReviewBoard(IRB)approvalwasnotobtainedforthisstudy,whichwasconductedbyKeltonGlobal,amarketresearchfirm,whoaccessedexistingparticipantpanelsacrosstheUS.
;allsubjectshadpreviouslyagreedtoparticipateinthenationalresearchpanelthatwasaccessed.
Additionally,allsubjectswereadvised,eitherverballyforphoneparticipation,orviaaninitialonlinescreenforInternetparticipationthat"Theresultsmayappearinleadingmediaoutletsinthecomingweeks,butyouranswerswillremainconfidentialandanonymous.
"ConsentforpublicationNotapplicableCompetinginterestsMEisanemployeeofKeltonGlobal.
AHAwasanemployeeandshareholderofPfizeratthetimeofthestudyanddevelopmentofthemanuscript.
BP,JCC,PH,andASarepaidemployeesandshareholdersofPfizer.
MMTisapracticingneurologistandreportsnoconflictsofinterest.
Publisher'sNoteSpringerNatureremainsneutralwithregardtojurisdictionalclaimsinpublishedmapsandinstitutionalaffiliations.
Authordetails1KeltonCommunications,CulverCity,CA,USA.
2PfizerInc.
,235East42ndStreet,NewYork,NY10017,USA.
3PfizerInc.
,Groton,CT,USA.
4PalmBeachNeurologicalCenter,PalmBeachGardens,FL,USA.
Received:23August2017Accepted:6December2017References1.
SadoskyA,McDermottAM,BrandenburgNA,StraussM.
Areviewoftheepidemiologyofpainfuldiabeticperipheralneuropathy,post-herpeticneuralgia,andlesscommonlystudiedneuropathicpainconditions.
PainPract.
2008;8(1):45–56.
2.
JambartS,AmmacheZ,HaddadF,YounesA,HassounA,AbdallaK,SelwanCA,SunnaN,WajsbrotD,YouseifE.
PrevalenceofpainfuldiabeticperipheralneuropathyamongpatientswithdiabetesmellitusintheMiddleEastregion.
JIntMedRes.
2011;39(2):366–77.
3.
AllemanCJ,WesterhoutKY,HensenM,ChambersC,StokerM,LongS,vanNootenFE.
HumanisticandeconomicburdenofpainfuldiabeticperipheralneuropathyinEurope:areviewoftheliterature.
DiabetesResClinPract.
2015;109(2):215–25.
4.
vanHeckeO,AustinSK,KhanRA,SmithBH,TorranceN.
Neuropathicpaininthegeneralpopulation:asystematicreviewofepidemiologicalstudies.
Pain.
2014;155(4):654–62.
5.
StewartWF,RicciJA,CheeE,HirschAG,BrandenburgN.
LostproductivetimeandcostsduetodiabetesanddiabeticneuropathicpainintheUSworkforce.
JOccupEnvironMed.
2007;49(6):672–9.
Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page8of96.
daCostaDiBonaventuraM,CappelleriJC,JoshiAV.
Alongitudinalassessmentofpainfuldiabeticperipheralneuropathyonhealthstatus,productivity,andhealthcareutilizationandcost.
PainMed.
2011;12(1):118–26.
7.
SadoskyA,MardekianJ,ParsonsB,HoppsM,BienenEJ,MarkmanJ.
Healthcareutilizationandcostsindiabetesrelativetotheclinicalspectrumofpainfuldiabeticperipheralneuropathy.
JDiabetesComplicat.
2015;29(2):212–7.
8.
SadoskyA,HopperJ,ParsonsB.
Painfuldiabeticperipheralneuropathy:resultsofasurveycharacterizingtheperspectivesandmisperceptionsofpatientsandhealthcarepractitioners.
Patient.
2014;7(1):107–14.
9.
PortenoyR.
Developmentandtestingofaneuropathicpainscreeningquestionnaire:IDpain.
CurrMedResOpin.
2006;22(8):1555–65.
10.
CleelandCS,RyanKM.
Painassessment:globaluseofthebriefpaininventory.
AnnAcadMedSingap.
1994;23(2):129–38.
11.
WorkProductivityandActivityImpairmentQuestionnaire:SpecificHealthProblemV2.
0(WPAI:SHP)[http://www.
reillyassociates.
net/WPAI_SHP.
html].
12.
ZelmanD,DukesE,BrandenburgN,BostromA,GoreM.
Identificationofcut-pointsformild,moderateandseverepainduetodiabeticperipheralneuropathy.
Pain.
2005;115(2):29–36.
13.
KleinbaumDG,KupperLL,NizamA,RosenbergES.
Appliedregressionanalysisandothermultivariatemethods.
5thed.
Boston:CengageLearning;2014.
14.
Rahim-WilliamsB,RileyJL3rd,WilliamsAK,FillingimRB.
Aquantitativereviewofethnicgroupdifferencesinexperimentalpainresponse:dobiology,psychology,andculturematterPainMed.
2012;13(4):522–40.
15.
HollingsheadNA,Ashburn-NardoL,StewartJC,HirshAT.
ThepainexperienceofHispanicAmericans:acriticalliteraturereviewandconceptualmodel.
JPain.
2016;17(5):513–28.
16.
KimH,NeubertJK,SanMiguelA,XuK,KrishnarajuRK,IadarolaMJ,GoldmanD,DionneRA.
Geneticinfluenceonvariabilityinhumanacuteexperimentalpainsensitivityassociatedwithgender,ethnicityandpsychologicaltemperament.
Pain.
2004;109(3):488–96.
17.
CampbellCM,EdwardsRR.
Ethnicdifferencesinpainandpainmanagement.
PainManag.
2012;2(3):219–30.
18.
NationalDiabetesStatisticsReport:EstimatesofDiabetesandItsBurdenintheUnitedStates,2014.
Atlanta:U.
S.
DepartmentofHealthandHumanServices.
http://www.
thefdha.
org/pdf/diabetes.
pdf.
19.
NationalHealthcareDisparitiesReport,2013.
Publication#14–0006[http://www.
ahrq.
gov/research/findings/nhqrdr/nhdr13/2013nhdr.
pdf].
20.
BetancourtJR,CorbettJ,BondarykMR.
Addressingdisparitiesandachievingequity:culturalcompetence,ethics,andhealth-caretransformation.
Chest.
2014;145(1):143–8.
Weacceptpre-submissioninquiriesOurselectortoolhelpsyoutondthemostrelevantjournalWeprovideroundtheclockcustomersupportConvenientonlinesubmissionThoroughpeerreviewInclusioninPubMedandallmajorindexingservicesMaximumvisibilityforyourresearchSubmityourmanuscriptatwww.
biomedcentral.
com/submitSubmityournextmanuscripttoBioMedCentralandwewillhelpyouateverystep:Eichholzetal.
ClinicalDiabetesandEndocrinology(2017)3:12Page9of9
- tests38ab.com相关文档
- 摇摇摇摇摇生态学报摇摇摇摇摇摇摇(SHENGTAI
- BRUCE38ab.com
- economic38ab.com
- amined38ab.com
- Healthiest38ab.com
- Figure38ab.com
美国服务器20G防御 50G防御 688元CN2回国
全球领先的IDC服务商华纳云“美国服务器”正式发售啦~~~~此次上线的美国服务器包含美国云服务器、美国服务器、美国高防服务器以及美国高防云服务器。针对此次美国服务器新品上线,华纳云也推出了史无前例的超低活动力度。美国云服务器低至3折,1核1G5M低至24元/月,20G DDos防御的美国服务器低至688元/月,年付再送2个月,两年送4个月,三年送6个月,且永久续费同价,更多款高性价比配置供您选择。...

HostKvm - 夏季云服务器七折优惠 香港和韩国机房月付5.95美元起
HostKvm,我们很多人都算是比较熟悉的国人服务商,旗下也有多个品牌,差异化多占位策略营销的,商家是一个创建于2013年的品牌,有提供中国香港、美国、日本、新加坡区域虚拟化服务器业务,所有业务均对中国大陆地区线路优化,已经如果做海外线路的话,竞争力不够。今天有看到HostKvm夏季优惠发布,主要针对香港国际和韩国VPS提供7折优惠,折后最低月付5.95美元,其他机房VPS依然是全场8折。第一、夏...

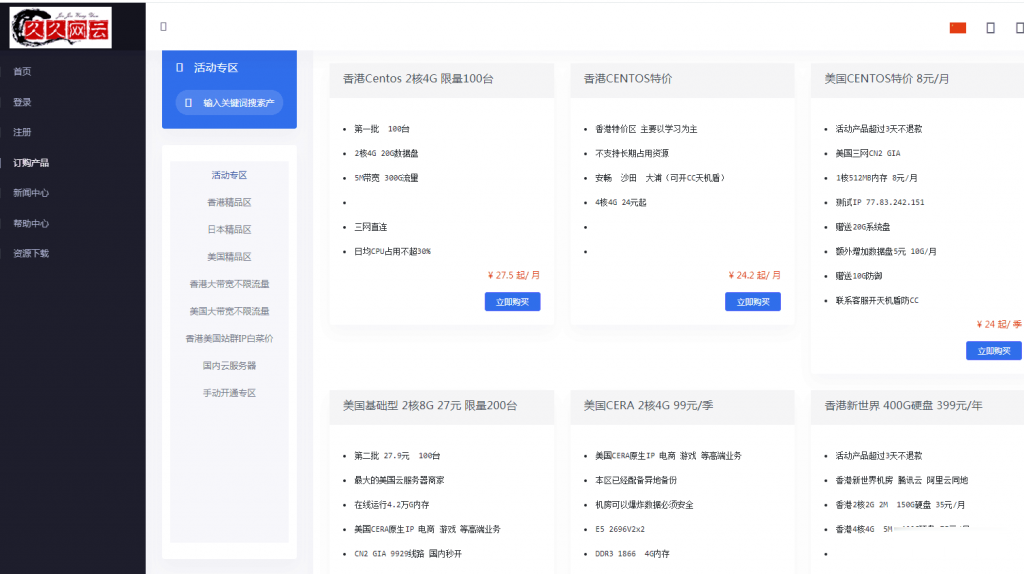
久久网云-目前最便宜的国内,香港,美国,日本VPS云服务器19.9元/月起,三网CN2,2天内不满意可以更换其他机房机器,IP免费更换!。
久久网云怎么样?久久网云好不好?久久网云是一家成立于2017年的主机服务商,致力于为用户提供高性价比稳定快速的主机托管服务,久久网云目前提供有美国免费主机、香港主机、韩国服务器、香港服务器、美国云服务器,香港荃湾CN2弹性云服务器。专注为个人开发者用户,中小型,大型企业用户提供一站式核心网络云端服务部署,促使用户云端部署化简为零,轻松快捷运用云计算!多年云计算领域服务经验,遍布亚太地区的海量节点为...
38ab.com为你推荐
-
存储备份数据备份有哪些方式呢?.cn域名cn域名和com域名有啥区别?各有啥优点?安徽汽车网在安徽那个市的二手车最好?同ip网站查询怎样查询一个ip绑了多少域名www.jjwxc.net在哪个网站看小说?8090lu.com8090lu.com怎么样了?工程有进展吗?www.mywife.ccmywife哪部最经典www.123qqxx.com我的首页http://www.hao123.com被改成了http://www.669dh.cn/?yhcename.com趫 是什么意思?干支论坛干支计时的干支计时