Mannheimcv狗狗
cv狗狗 时间:2021-05-25 阅读:()
Toometal.
ActaVetScand(2016)58:46DOI10.
1186/s13028-016-0228-1CASEREPORTInterstitialpneumoniaandpulmonaryhypertensionassociatedwithsuspectedehrlichiosisinadogMarjoleinLisettedenToom1*,TetydaPaulinaDobak2,ElsMarionBroens3andChiaraValtolina1AbstractBackground:Indogswithcaninemonocyticehrlichiosis(CME),respiratorysignsareuncommonandclinicalandradiographicsignsofinterstitialpneumoniaarepoorlydescribed.
However,inhumanmonocyticehrlichiosis,respira-torysignsarecommonandsignsofinterstitialpneumoniaarewellknown.
Pulmonaryhypertension(PH)isclassifiedbasedontheunderlyingdiseaseanditstreatmentisaimedatreducingtheclinicalsignsand,ifpossible,addressingtheprimarydiseaseprocess.
PHisoftenirreversible,butcanbereversibleifitissecondarytoatreatableunderlyingetiology.
CMEiscurrentlynotgenerallyrecognizedasoneofthepossiblediseasesleadingtointerstitialpneumoniaandsecondaryPHindogs.
OnlyonecaseofPHassociatedwithCMEhasbeenreportedworldwide.
Casepresentation:Aseven-year-old,maleintact,mixedbreeddogwaspresentedwith2weekshistoryoflethargyanddyspnea.
ThedogpreviouslylivedintheCapeVerdeanislands.
Physicalexaminationshowedsignsofright-sidedcongestiveheartfailureandpoorperipheralperfusion.
Thoracicradiographyshowedmoderateright-sidedcardio-megalywithdilationofthemainpulmonaryarteryandamilddiffuseinterstitiallungpatternwithperibronchialcuff-ing.
Echocardiographyshowedseverepulmonaryhypertensionwithanestimatedpressuregradientof136mmHg.
Onarterialbloodgasanalysis,severehypoxemiawasfoundandcompletebloodcountrevealedmoderateregenera-tiveanemiaandseverethrombocytopenia.
Aseveregammahyperglobulinemiawasalsodocumented.
SerologyforEhrlichiacaniswashighlypositive.
Treatmentwithoxygensupplementation,atypedpackedredbloodcelltransfu-sionandmedicaltherapywithdoxycycline,pimobendanandsildenafilwasinitiatedandthedogimprovedclinically.
Approximately2weekslater,therewascompleteresolutionofallclinicalsignsandmarkedimprovementofthePH.
Conclusion:ThisreportillustratesthatCMEmightbeassociatedwithsignificantpulmonarydiseaseandshouldbeconsideredasapossibledifferentialdiagnosisindogspresentingwithdyspneaandsecondarypulmonaryhyperten-sion,especiallyindogsthathavebeeninendemicareas.
ThisisimportantbecauseCMEisatreatablediseaseanditssecondarylungandcardiacmanifestationsmaybecompletelyreversible.
Keywords:Canine,Ehrlichiosis,Pulmonaryhypertension,Reversible,Interstitiallungdisease2016denToometal.
ThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
BackgroundEhrlichiacanisisapleomorphicbacteriumthatinfectscirculatingmonocytesandcancausecaninemono-cyticehrlichiosis(CME).
CMEresultsinvariablenon-specificclinicalmanifestationsandclinicalsignscanbesubclinical,acuteorchronic.
Mostdogspresentwithdepression,lethargy,mildweightloss,anorexia,splenomegaly,andlymphadenopathywithorwithouthemorrhagictendencies[1,2].
Respiratorysignsarespo-radicallyreportedindogsbutareregularlydescribedinhumanpatientsinfectedwithhumanmonocyticehrli-chiosis(HME)[3].
Interstitialpneumoniacanhaveaninfectiousornon-infectiousetiology.
Indogs,reportedinfectiousagentsleadingtointerstitialpneumoniaareAngiostrongylusOpenAccessActaVeterinariaScandinavica*Correspondence:M.
L.
denToom@uu.
nl1DepartmentofClinicalSciencesofCompanionAnimals,FacultyofVeterinaryMedicine,UtrechtUniversity,Yalelaan108,3508TDUtrecht,TheNetherlandsFulllistofauthorinformationisavailableattheendofthearticlePage2of8Toometal.
ActaVetScand(2016)58:46vasorum,Leishmaniachagasi,Toxoplasmagondii,Pneumocystiscarinii,Babesiacanis,Leptospirasp.
,Mycoplasmasp,caninedistempervirusandadenovi-rus[4–12].
Inpatientswithinterstitialpneumonia,gasexchangeisoftenimpairedduetoventilation-perfusionmismatching,intrapulmonaryshunting,anddecreaseddiffusionacrosstheabnormalinterstitiumwitharterialhypoxiaasaconsequence.
Incontrasttothesystemicvasculaturethatrespondswitharterialvasodilationtobetterperfusehypoxictissue,thepulmonaryvasculatureconstrictsinresponsetohypoxia.
Besidespulmonaryvasoconstriction,hypoxiaalsocausesproliferationofthesmoothmusclecellsinthearterialwall.
Bothphenom-enaleadtoadecreaseinluminalcross-sectionalareaandanincreaseinpulmonaryvascularresistanceindexwithpulmonaryhypertension(PH)asaconsequence.
Pulmonaryhypertensionisclassifiedbasedontheunderlyingdiseaseanditstreatmentisaimedatimprov-ingtheclinicalsignsandaddressingtheprimarydiseaseprocess[13].
AlthoughPHisoftenirreversible,PHisreversibleinsomecasesiftheunderlyingetiologyisdiag-nosedandtreatedaccordingly.
ReversibilityofPHhasforinstancebeendemonstratedindogsaftersuccessfultreatmentforA.
vasorum[14].
Pulmonarychangesconsistentwithinterstitialpneu-moniahavebeenreportedpreviouslyinhumanswithHME[3]andasanatypicalfindingindogswithCME[15–18].
However,CMEisgenerallynotrecognizedasoneofthepossiblediseasesleadingtointerstitialpneu-moniaandsecondaryPHindogs.
OnlyonecaseofPHassociatedwithE.
canisinfectionhasbeenreportedworldwide[19].
Consequently,CMEmightbeunderdiag-nosedasapossiblecauseofinterstitialpneumoniaandsecondaryPH.
Thiscasereportdescribestheclinical,radiographicandechocardiographicpresentationofadogwithinter-stitialpneumoniaandseverePHsuspectedtobeassoci-atedwithE.
canisinfection.
CasepresentationAseven-year-old,intactmale,mixedbreeddogweigh-ing8.
1kgwaspresentedtotheEmergencyServiceoftheDepartmentofClinicalScienceofCompanionAni-malsoftheFacultyofVeterinaryMedicine,UtrechtUniversitywitha2weekshistoryoflethargy,progres-sivedyspneaandcoughing.
ThedogpreviouslylivedintheCapeVerdeanislandsforapproximately3yearsandreturnedtotheNetherlands10monthsbeforepresenta-tion.
Inthepast2years,thedoghadshowedchronicmildexerciseintoleranceandhadafewepisodesofdiarrheathatresolvedwithsymptomatictherapy.
Thedogwasup-todatewithhisvaccinationsandanthel-minthictreatments.
Physicalexaminationshowedgeneralizedweaknessanddecreasementalstate.
Cardiovascularexamina-tionrevealedtachycardia,weakperipheralpulses,palemucousmembranes,prolongedcapillaryrefilltime,jugu-lardistensionsandvenouspulses,andagradethreeoutofsixsystolicmurmurwiththepointofmaximalinten-sityovertherightcardiacapex.
Thedogwasalsoseverelydyspneicanddemonstratedharshlungsoundsonauscul-tation.
Theabdomenwasdistendedandpositiveundula-tionwasdetected.
Thesefindingswereconsistentwithpulmonarydisease,right-sidedheartfailureandpoorperipheralperfusion.
Completebloodcount(CBC)showedamoderatemicrocytic,hypochromicanemia,moderateleukocyto-siswithamarkedleftshiftandaseverethrombocyto-penia.
Biochemistryshowedseverehyperproteinemia,hyperglobulinemiaandamildhypoalbuminemia.
Serumproteinelectrophoresisshowedapolyclonalpeakinthegammaglobulinregion.
Arterialbloodgasanalysisshowedaseverehypoxemiawithhypocapnia.
Urinaly-sisshowedmildhemoglobinuria,glucosuriaandpro-teinuria.
Bloodsamplesweresubmittedforserologicalandmolecularbiologicaltesting.
Immunofluorescenceantibodytest(IFAT)forE.
canis(MegaFLUOEhrlichiacanis,MegaCorDiagnostikGmbH,Hrbranz,Aus-tria)waspositive(IgGtiter>2560),butpolymerasechainreaction(PCR)amplificationforEhrlichiagenus(real-timePCR,LightCycler2.
0,RocheDiagnosticsGmBH,Mannheim,Germany,primersusedasdescribedprevi-ously[20])wasnegative.
SerologyforLeishmaniasp.
(Dog-DAT,Leishmaniaspecificantibodydetectionkit,KoninklijkInstituutvoordeTropen,Amsterdam,theNetherlands)andB.
canis.
(MegaFLUOBabesiscanis,MegaCorDiagnostikGmbH,Hrbranz,Austria)andantigensnaptestsforA.
vasorum(AngioDetectTest,IDEXXLaboratories)andDirofilariaimmitis(SNAPHeartwormRTTest,IDEXXLaboratories)werealsoneg-ative.
LaboratoryresultsaresummarizedinTable1.
Onthoracicradiographs,amilddiffuseincreaseinpulmonaryopacitywithaninterstitiallungpatternandmildperibronchialcuffingwasseen,whichwasmostaccentuatedinthecaudodorsallunglobes.
Thinpleuralfissurelineswerenotedbetweenalllunglobes.
Thecar-diacsilhouetteshowedsignsofright-sidedcardiomegaly(vertebralheartscore(VHS):11.
0,referenceinterval75mmHg)[13],(Fig.
3).
ToaddresstheseverehypoxemiaandPHthedogwasplacedinanoxygencagewithaninspiredconcentra-tionofoxygenbetween40and50%.
Theclinicalsignsofthedogdidnotimprovemarkedlywiththeextraoxygensupplementation.
Becauseanemiacouldhavecontributedtothecardiovascularsignsandthepoortis-sueoxygenation,atypedpackedredbloodcelltransfu-sionwasadministered.
Basedonthetravelhistory,theabnormalitieswithintheCBCandbiochemicalanalysisandthepositiveserologyforE.
canis,aninfectionwithCMEwassuspected.
Treatmentwithdoxycycline(5mg/kg,orallytwicedaily)(Doxoral,ASTFarma,Oudewa-ter,theNetherlands),pimobendan(0.
3mg/kg,orallytwicedaily)(CardisureFlavour,EurovetAnimalHealthBV,Bladel,theNetherlands)andsildenafil(1.
5mg/kg,orallytwicedaily)(Viagra,Pfizer,NewYork,USA)wasinitiated.
Thehematocritincreasedfrom20to36%afterthebloodtransfusionandthedog'sclinicalconditionimprovedremarkably.
However,thedogremainedmod-eratelydyspneicandseverelyhypoxic(PaO2:46.
5mmHg,referenceinterval:85.
0–103.
3mmHg).
Thedyspneagraduallyimprovedandthedogseemedcomfortableout-sidetheoxygencageafter6daysoftreatment,althoughtheimprovementofthehypoxemiawasonlyminimal(PaO2:55mmHg,referenceinterval:85–103.
3mmHg,Table1).
Becauseoffinanciallimitationsoftheowner,thedogwasdischargedwiththeabove-mentionedthera-piesatthattime.
Seventeendaysafterinitiationoftreatment,thedogwasadmittedviathecardiologypolyclinicsofthesameuni-versityandre-examined.
Atthattime,therewascompleteresolutionofallclinicalsignsandphysicalexaminationwascompletelyunremarkable.
CBCshowednormalplate-letcountsandleukogram,withonlyaverymildmicrocytichypochromicanemia.
Biochemicalanalysisagainshowedseverehyperproteinemiaandhyperglobulinemia.
TheTable1Summaryofhaematological,biochemical,serologicalandurineandbloodgasanalysisresultsArterialbloodgasanalysiswasperformedwithaninspiredconcentrationofoxygenof21%ValuesinitalicsareoutsidethereferenceintervalMCVmeancorpuscularvolume,MCHCmeancorpuscularhemoglobinconcentration,MCHmeancorpuscularhemoglobin,WBCwhitebloodcellcount,UPCurinaryproteintocreatinineratio,PaO2partialarterialoxygenpressure,PaCO2partialarterialcarbondioxidepressure,BEbaseexcessParameterDay1Day7Day17Day50ReferenceintervalHematocrit(L/L)0.
200.
380.
400.
340.
42–0.
61MCV(fl)57.
759.
959.
963.
5–72.
9MCHC(mmol/L)21.
721.
822.
220.
5–22.
4MCH(fmol)1.
251.
311.
331.
37–1.
57TotalWBC(*109/L)23.
16.
66.
74.
5–14.
6Segmentedneutrophils(*109/L)17.
32.
64.
42.
9–11.
0Bandneutrophils(*109/L)3.
20.
00.
00.
0–0.
3Lymphocytes(*109/L)2.
13.
01.
80.
8–4.
7Monocytes(*109/L)0.
50.
40.
30.
0–0.
9Eosinophils(*109/L)0.
00.
50.
20.
0–1.
6Platelets(*109/L)15251166144–603Urea(mmol/L)4.
17.
03.
0–12.
5Creatinine(mol/L)33747750–129Sodium(mmol/L)145145141141–150Potassium(mmol/L)4.
14.
73.
73.
6–5.
6Totalprotein(g/L)911198955–72Albumin(g/L)16272626–37Gamma-globulins(g/L)5768403–9UPC0.
80.
31:25601:256040areconsideredpositiveforE.
canisexposure[21].
InFig.
3Echocardiographicimagesatpresentationfromleftapical4-chamberview.
acolorDopplermapofseveretricuspidregurgitation.
RArightatrium,RVrightventricle,LAleftatrium,LVleftventricle.
bspectralDopplertraceoftricuspidregurgitation.
Tricuspidsystolicvelocityof5.
8m/s,indi-catingapeaktricuspidpressuregradientofapproximately136mmHg,gradedasseverepulmonaryhypertension(reference75mmHgFig.
4Rightlateral(a)anddorsoventral(b)thoracicradiographs2weeksafterdischarge.
Radiographsdemonstratingresolutionofcardiomegaly(vertebralheartscore:10.
2,referenceinterval2560),whichstrength-enedthesuspicionofanactiveinfection[22].
However,definiteactiveinfectionatthetimeofpres-entationcouldnotbeproven,becausePCRamplifica-tionforEhrlichiagenuswasnegativeandanti-EhrlichialIgGantibodiespersistforseveralmonthstoyearsaftereliminationoftheparasite[23].
AnegativeresultfromaPCRtestcanoccurwhenorganismsincirculationarebelowthelevelofdetection,asmayhappenwheninfec-tionsarechronic.
IthasbeendemonstratedthatdogscanbePCRnegativeonbloodsamples,butPCRpositiveonsplenicaspirates[21].
ItishypothesizedthattheE.
canisaresequesteredinsplenicmacrophagestoavoidimmuneelimination.
Unfortunately,inthepresentcase,theown-ersdeclinedfineneedleaspiratesofthespleenduetothepotentialrisksandstressinvolved,e.
g.
internalbleeding,aggravationofthedyspnea.
Pairedserologysamplescanalsoprovideusefulinformationaboutantibodykinetics,whichmaypointtocurrentstatusofinfection.
Afour-foldincreaseinIgGantibodiesovertimeissuggestedtobeevidenceforanactiveinfection[24].
Antibodytiterswilldecreasegraduallyafterappropriatetreatment,butmaypersistformonthstoyearsevenafterfullclini-calrecovery[23,25].
Inthiscase,theEhrlichiaIgGtiterwasstillveryhigh17daysafterinitiationofdoxycyclinetherapy,probablyduetotheshorttimebetweenstartofthetreatmentandretesting;IFATwasunfortunatelynotrepeatedonday50.
Althoughdoxycyclinetherapygenerallyresultsinfastclinicalimprovementandimprovementofmostlabora-toryabnormalities,persistenceofhyperglobulinemiaisgenerallyobservedforalongerperiod.
Moststudieshaveshownnormalizationofserumproteinelectrophoresisresultsafter3–9monthsoftherapy[1,15].
Thisexplainsthepersistenceofhyperglobulinemiaatthere-examina-tionsofthedogatdays17and50.
Inhumanmedicine,respiratorysignsarecommonlydescribedasaconsequenceofHMEinfection[3]andacuterespiratorydistresssyndrome(ARDS)hasalsobeenreportedasasevere,althoughuncommon,findinginHME[26–28].
BothCMEandHMEanimalmodelsalsorevealedprominentmononuclearcellularinfiltrationintheinteralveolarsepta,endothelialdamageandvasculi-tisinthelungs[16,29].
Thiscouldexplainthepulmonarychangesfoundinthisdogandtheclinicalandradio-graphicimprovementaftertreatmentwithdoxycycline.
However,recently,acuteresolutionofpatchypulmonaryalveolarinfiltrateshasbeendescribedaftersildenafiltherapyindogswithidiopathicPHandPHsecondarytoidiopathiclungfibrosis[30].
Therefore,sildenafiltherapymightalsohavecontributedtotheimprovementoftheradiographicchangesinthiscase.
AnotherexplanationFig.
5Echocardiographicimagesobtained2weeksaftertreatmentfromrightparasternalshortaxisview.
a,b:Two-dimensional(a)andM-mode(b)viewdemonstratingnormalizationofcardiacdimensionsandfunction.
cTwo-dimensionalviewofpulmonaryartery(PA)andaorta(AO).
ThePAisuniformlyminimallydilatedwithaPA/Aoratioof1.
2(referenceinterval:0.
8–1.
15)Page7of8Toometal.
ActaVetScand(2016)58:46fortheradiographicabnormalitiesandtheimprovementondoxycyclinetherapythatcannotbeexcludedisthatthedogsufferedfromabacterialpneumonia.
Furthermore,animportantpossiblefactorthatmighthavecontributedtothehypoxemiaandPHinthisdogispulmonarythromboembolism(PTE)[31].
PTEcanoccurascomplicatingsequelaeinpatientswithPHorcanbetheprimarycauseofPH[32].
Inpeople,itisincreasinglyrecognizedthatpatientswithpulmonaryarterialhypertensionhavedysregulatedcoagulationandantithrombotichomeostasis,whichmaycontributetoaprothromboticstate[33].
Unfortunately,wedidnotperformdiagnosticinvestigationssuchasD-dimercon-centration[34],computedtomographypulmonaryangi-ography[35]orthromboelastography(TEG)[36,37]toinvestigateifthedogsufferedfromPTEoraprothrom-boticstate.
However,totheauthor'sknowledge,PTEhasneverbeenassociatedwithCMEinveterinaryliterature.
OnlytwocasesofaorticandportalveinthrombosishavebeendescribedindogswithCME[38,39].
TreatmentofPHisaimedateliminatingorimprovingtheunderlyingdiseaseprocess.
IfthePHisnotcontrolledbyprimarydiseasetherapyorifthePHisidiopathic,treatmentwithpulmonaryarterialdilatorsmaybeimple-mented.
Inveterinarymedicinecurrently,onlyphos-phodiesteraseinhibitorsareused.
Sildenafilisahighlyselectivephosphodiesterasefiveinhibitorthathasbeenusedinveterinarymedicinewithencouragingresults[30,40].
Pimobendan,acalcium-sensitizingagentwithphosphodiesterasethreeinhibitingactionshasalsobeenused,especiallywhenleftheartdiseaseisacontributingcause[41].
Inthepresentcase,adualtherapywithpul-monaryarterialdilatorswasinitiated,becausewehopedthiswouldamelioratetheveryseverePHandclinicalsignsfasterthanamonotherapywithsildenafil.
Althoughrecoveryhasbeendescribedinasimilarcasewithjustamonotherapywithdoxycycline[19],webelievethatthesymptomaticsupportwithpulmonaryvasodilatorswasjustifiedinthisdog.
MildtomoderateimprovementoftricuspidregurgitationgradientbysildenafiltherapyhasbeendescribedinsomedogswithPH[30],butnotinothers[42].
Consequently,wecannotruleoutthattheimprovementoftheechocardiographicchangescouldalsobepartiallyexplainedbytheuseofthevasodilatingdrugs.
Ideally,anotherechocardiogramshouldhavebeenperformedafterdiscontinuationofthevasodilatorther-apy.
However,theimprovementwassodramatic,thatwedonotbelievethatthiscouldbesolelyexplainedbythevasodilatortherapy.
ThiscasereportillustratesthatCMEmightbeasso-ciatedwithsignificantpulmonarydiseaseandthatitshouldbeconsideredasapossibledifferentialdiag-nosisindogspresentingwithdyspneaandsecondarypulmonaryhypertension,especiallyindogsthathavebeeninendemicareas.
ThisisimportantbecauseCMEisatreatablediseaseanditslungandcardiacmanifesta-tionsmaybecompletelyreversible.
Authors'contributionsCVperformedtheinitialclinicalinvestigationsofthedogandwasresponsibleforthecareandtreatmentofthedogduringadmittanceattheIntensiveCareUnit.
EBwasresponsiblefortheserologicalandmolecularbiologicaldiagnostictesting.
MDTalsoperformedclinicalinvestigationsofthedogandperformedandevaluatedtheechocardiogramsofthedogduringhospitaliza-tionandatfollow-up.
TDperformedandevaluatedtheinitialechocardiogramofthedogatpresentationandwasresponsiblefortheinterpretationofthethoracicradiography.
ThemanuscriptwasdraftedbyMDTandfinalizedjointlybyallauthors.
Allauthorsreadandapprovedthefinalmanuscript.
Authordetails1DepartmentofClinicalSciencesofCompanionAnimals,FacultyofVeterinaryMedicine,UtrechtUniversity,Yalelaan108,3508TDUtrecht,TheNetherlands.
2DepartmentofDiagnosticImaging,FacultyofVeterinaryMedicine,UtrechtUniversity,Yalelaan108,3508TDUtrecht,TheNetherlands.
3DepartmentofInfectiousDiseasesandImmunology,FacultyofVeterinaryMedicine,Utre-chtUniversity,POBox80.
165,3508TDUtrecht,TheNetherlands.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Received:19March2016Accepted:30June2016References1.
Sainz,RouraX,MiróG,EstradaPeaA,KohnB,HarrusS,etal.
GuidelineforveterinarypractitionersoncanineehrlichiosisandanaplasmosisinEurope.
ParasitVectors.
2015;8:75.
2.
LittleSE.
Ehrlichiosisandanaplasmosisindogsandcats.
VetClinNorthAmSmallAnimPract.
2010;40:1121–40.
3.
EngTR,HarkessJR,FishbeinDB,DawsonJE,GreeneCN,RedusMA,etal.
Epidemiologic,clinical,andlaboratoryfindingsofhumanehrlichiosisintheUnitedStates,1988.
JAMA.
1990;264:2251–8.
4.
PandherK,PodellB,GouldDH,JohnsonBJ,ThompsonS.
Interstitialpneumoniainneonatalcaninepupswithevidenceofcaninedistempervirusinfection.
JVetDiagnInvest.
2006;18:201–4.
5.
GonalvesR,TafuriW,deMeloM,RasoP.
Chronicinterstitialpneumo-nitisindogsnaturallyinfectedwithLeishmania(Leishmania)chagasi:ahistopathologicalandmorphometricstudy.
RevInstMedTropSaoPaulo.
2003;45:153–8.
6.
KirbergerRM,LobettiRG.
RadiographicaspectsofPneumocystiscariniipneumoniaintheminiatureDachshund.
VetRadiolUltrasound.
1998;39:313–7.
7.
HongS,KimO.
MolecularidentificationofMycoplasmacynosfromlaboratorybeagledogswithrespiratorydisease.
LabAnimRes.
2012;28:61–6.
8.
GendronK,ChristeA,WalterS,SchweighauserA,FranceyT,DoherrMG,etal.
SerialCTfeaturesofpulmonaryleptospirosisin10dogs.
VetRec.
2014;174:169.
9.
DasteT,LucasM,AumannM.
Cerebralbabesiosisandacuterespiratorydistresssyndromeinadog.
JVetEmergCritCare.
2013;23:615–23.
10.
BorgeatK,SudunaguntaS,KayeB,SternJ,LuisFuentesV,ConnollyDJ.
Retrospectiveevaluationofmoderate-to-severepulmonaryhypertensionindogsnaturallyinfectedwithAngiostrongylusvasorum.
JSmallAnimPract.
2015;56:196–202.
11.
CastlemanWL.
Bronchiolitisobliteransandpneumoniainducedinyoungdogsbyexperimentaladenovirusinfection.
AmJPathol.
1985;119:495–504.
12.
CapenCC,ColeCR.
Pulmonarylesionsindogswithexperimentalandnaturallyoccurringtoxoplasmosis.
PatholVet.
1966;3:40–63.
Page8of8Toometal.
ActaVetScand(2016)58:4613.
KellihanH,StepienR.
Pulmonaryhypertensionindogs:diagnosisandtherapy.
VetClinNorthAmSmallAnimPract.
2010;40:623–41.
14.
EstèvesI,TessierD,DandrieuxJ,PolackB,CarlosC,BoulangerV,etal.
Reversiblepulmonaryhypertensionpresentingsimultaneouslywithanatrialseptaldefectandangiostrongylosisinadog.
JSmallAnimPract.
2004;45:206–9.
15.
NeerTM,BreitschwerdtE,GreeneR,LappinM.
ConsensusstatementonehrlichialdiseaseofsmallanimalsfromtheinfectiousdiseasestudygroupoftheACVIM.
AmericanCollegeofVeterinaryInternalMedicine.
JVetInternMed.
2002;16:309–15.
16.
SotomayorEA,PopovVL,FengHM,WalkerDH,OlanoJP.
Animalmodeloffatalhumanmonocytotropicehrlichiosis.
AmJPathol.
2001;158:757–69.
17.
FrankJR,BreitschwerdtEB.
Aretrospectivestudyofehrlichiosisin62dogsfromNorthCarolinaandVirginia.
JVetInternMed.
1999;13:194–201.
18.
CodnerEC,RobertsRE,AinsworthAG.
Atypicalfindingsin16casesofcanineehrlichiosis.
JAmVetMedAssoc.
1985;186:166–9.
19.
LocatelliC,StefanelloD,RiscazziG,BorgonovoS,ComazziS.
PulmonaryhypertensionassociatedwithEhrlichiacanisinfectioninadog.
VetRec.
2012;170:676.
20.
BekkerCPJ,deVosS,TaoufikA,SparaganoOAE,JongejanF.
SimultaneousdetectionofAnaplasmaandEhrlichiaspeciesinruminantsanddetectionofEhrlichiaruminantiuminAmblyommavariegatumticksbyreverselineblothybridization.
VetMicrobiol.
2002;89:223–38.
21.
HarrusS,WanerT.
Diagnosisofcaninemonocytotropicehrlichiosis(Ehrli-chiacanis):anoverview.
VetJ.
2011;187:292–6.
22.
WenB,RikihisaY,MottJM,GreeneR,KimHY,ZhiN,etal.
ComparisonofnestedPCRwithimmunofluorescent-antibodyassayfordetectionofEhrlichiacanisinfectionindogstreatedwithdoxycycline.
JClinMicrobiol.
1997;35:1852–5.
23.
BartschRC.
Post-therapyantibodytitersindogswithehrlichiosis:follow-upstudyon68patientstreatedprimarilywithtetracyclineand/ordoxycycline.
JVetInternMed.
1996;10:271–4.
24.
WanerT,HarrusS,JongejanF,BarkH,KeysaryA,CornelissenAW.
Signifi-canceofserologicaltestingforehrlichialdiseasesindogswithspecialemphasisonthediagnosisofcaninemonocyticehrlichiosiscausedbyEhrlichiacanis.
VetParasitol.
2001;95:1–15.
25.
IqbalZ,RikihisaY.
ReisolationofEhrlichiacanisfrombloodandtissuesofdogsafterdoxycyclinetreatment.
JClinMicrobiol.
1994;32:1644–9.
26.
WeaverRA,VirellaG,WeaverA.
Ehrlichiosiswithseverepulmonarymani-festationsdespiteearlytreatment.
SouthMedJ.
1999;92:336–9.
27.
PatelRG,ByrdMA.
Nearfatalacuterespiratorydistresssyndromeinapatientwithhumanehrlichiosis.
SouthMedJ.
1999;92:333–5.
28.
MutnejaR,ShahM,ShivamurthyP,GowaniS,DelgadoColonD,LawlorM.
Acuterespiratorydistresssyndromeinhumangranulocyticehrlichiosis.
ConnMed.
2014;78:345–7.
29.
ReardonMJ,PierceKR.
Acuteexperimentalcanineehrlichiosis.
II.
Sequen-tialreactionofthehemicandlymphoreticularsystemofselectivelyimmunosuppresseddogs.
VetPathol.
1981;18:384–95.
30.
KellihanH,WallerK,PinkosA,SteinbergH,BatesM.
Acuteresolutionofpulmonaryalveolarinfiltratesin10dogswithpulmonaryhypertensiontreatedwithsildenafilcitrate:2005–2014.
JVetCardiol.
2015;17:182–91.
31.
GoggsR,BenigniL,FuentesV,ChanD.
Pulmonarythromboembolism.
JVetEmergCritCare.
2009;19:30–52.
32.
GalieN,HumbertM,VachieryJL,GibbsS,LangI,TorbickiA,etal.
2015ESC/ERSGuidelinesforthediagnosisandtreatmentofpulmonaryhyper-tension:thejointtaskforceforthediagnosisandtreatmentofpulmonaryhypertensionoftheEuropeansocietyofcardiology(ESC)andtheEuropeanrespiratorysociety(ERS):endorsedby:associationforEuropeanpaediatricandcongenitalcardiology(AEPC),Internationalsocietyforheartandlungtransplantation(ISHLT).
EurHeartJ.
2016;37:67–119.
33.
RoldanT,LandzbergMJ,DeicicchiDJ,AtayJK,WaxmanAB.
Anticoagula-tioninpatientswithpulmonaryarterialhypertension:anupdateoncurrentknowledge.
JHeartLungTransplant.
2016;35:151–64.
34.
EpsteinSE,HopperK,MellemaMS,JohnsonLR.
DiagnosticutilityofD-dimerconcentrationsindogswithpulmonaryembolism.
JVetInternMed.
2013;27:1646–9.
35.
GoggsR,ChanDL,BenigniL,HirstC,KellettGregoryL,FuentesVL.
Comparisonofcomputedtomographypulmonaryangiographyandpoint-of-caretestsforpulmonarythromboembolismdiagnosisindogs.
JSmallAnimPract.
2014;55:190–7.
36.
GoggsR,WiinbergB,Kjelgaard-HansenM,ChanDL.
Serialassessmentofthecoagulationstatusofdogswithimmune-mediatedhaemolyticanaemiausingthromboelastography.
VetJ.
2012;191:347–53.
37.
KolA,BorjessonDL.
Applicationofthrombelastography/thromboelasto-metrytoveterinarymedicine.
VetClinPathol.
2010;39:405–16.
38.
BresslerC,HimesLC,MoreauRE.
PortalveinandaorticthrombosesinaSiberianhuskywithehrlichiosisandhypothyroidism.
JSmallAnimPract.
2003;44:408–10.
39.
LambCR,WrighleyRH,SimpsonKW,HijfteMF,GardenOA,SmythJBA,etal.
Ultrasonographicdiagnosisofportalveinthrombosisinfourdogs.
VetRadiolUltrasoun.
1996;37:121–9.
40.
BrownAJ,DavisonE,SleeperMM.
Clinicalefficacyofsildenafilintreat-mentofpulmonaryarterialhypertensionindogs.
JVetInternMed.
2010;24:850–4.
41.
AtkinsonKJ,FineDM,ThombsLA,GorelickJJ,DurhamHE.
EvaluationofpimobendanandN-terminalprobrainnatriureticpeptideinthetreat-mentofpulmonaryhypertensionsecondarytodegenerativemitralvalvediseaseindogs.
JVetInternMed.
2009;23:1190–6.
42.
KellumH,StepienR.
Sildenafilcitratetherapyin22dogswithpulmonaryhypertension.
JVetInternMed.
2007;21:1258–64.
ActaVetScand(2016)58:46DOI10.
1186/s13028-016-0228-1CASEREPORTInterstitialpneumoniaandpulmonaryhypertensionassociatedwithsuspectedehrlichiosisinadogMarjoleinLisettedenToom1*,TetydaPaulinaDobak2,ElsMarionBroens3andChiaraValtolina1AbstractBackground:Indogswithcaninemonocyticehrlichiosis(CME),respiratorysignsareuncommonandclinicalandradiographicsignsofinterstitialpneumoniaarepoorlydescribed.
However,inhumanmonocyticehrlichiosis,respira-torysignsarecommonandsignsofinterstitialpneumoniaarewellknown.
Pulmonaryhypertension(PH)isclassifiedbasedontheunderlyingdiseaseanditstreatmentisaimedatreducingtheclinicalsignsand,ifpossible,addressingtheprimarydiseaseprocess.
PHisoftenirreversible,butcanbereversibleifitissecondarytoatreatableunderlyingetiology.
CMEiscurrentlynotgenerallyrecognizedasoneofthepossiblediseasesleadingtointerstitialpneumoniaandsecondaryPHindogs.
OnlyonecaseofPHassociatedwithCMEhasbeenreportedworldwide.
Casepresentation:Aseven-year-old,maleintact,mixedbreeddogwaspresentedwith2weekshistoryoflethargyanddyspnea.
ThedogpreviouslylivedintheCapeVerdeanislands.
Physicalexaminationshowedsignsofright-sidedcongestiveheartfailureandpoorperipheralperfusion.
Thoracicradiographyshowedmoderateright-sidedcardio-megalywithdilationofthemainpulmonaryarteryandamilddiffuseinterstitiallungpatternwithperibronchialcuff-ing.
Echocardiographyshowedseverepulmonaryhypertensionwithanestimatedpressuregradientof136mmHg.
Onarterialbloodgasanalysis,severehypoxemiawasfoundandcompletebloodcountrevealedmoderateregenera-tiveanemiaandseverethrombocytopenia.
Aseveregammahyperglobulinemiawasalsodocumented.
SerologyforEhrlichiacaniswashighlypositive.
Treatmentwithoxygensupplementation,atypedpackedredbloodcelltransfu-sionandmedicaltherapywithdoxycycline,pimobendanandsildenafilwasinitiatedandthedogimprovedclinically.
Approximately2weekslater,therewascompleteresolutionofallclinicalsignsandmarkedimprovementofthePH.
Conclusion:ThisreportillustratesthatCMEmightbeassociatedwithsignificantpulmonarydiseaseandshouldbeconsideredasapossibledifferentialdiagnosisindogspresentingwithdyspneaandsecondarypulmonaryhyperten-sion,especiallyindogsthathavebeeninendemicareas.
ThisisimportantbecauseCMEisatreatablediseaseanditssecondarylungandcardiacmanifestationsmaybecompletelyreversible.
Keywords:Canine,Ehrlichiosis,Pulmonaryhypertension,Reversible,Interstitiallungdisease2016denToometal.
ThisarticleisdistributedunderthetermsoftheCreativeCommonsAttribution4.
0InternationalLicense(http://creativecommons.
org/licenses/by/4.
0/),whichpermitsunrestricteduse,distribution,andreproductioninanymedium,providedyougiveappropriatecredittotheoriginalauthor(s)andthesource,providealinktotheCreativeCommonslicense,andindicateifchangesweremade.
TheCreativeCommonsPublicDomainDedicationwaiver(http://creativecommons.
org/publicdomain/zero/1.
0/)appliestothedatamadeavailableinthisarticle,unlessotherwisestated.
BackgroundEhrlichiacanisisapleomorphicbacteriumthatinfectscirculatingmonocytesandcancausecaninemono-cyticehrlichiosis(CME).
CMEresultsinvariablenon-specificclinicalmanifestationsandclinicalsignscanbesubclinical,acuteorchronic.
Mostdogspresentwithdepression,lethargy,mildweightloss,anorexia,splenomegaly,andlymphadenopathywithorwithouthemorrhagictendencies[1,2].
Respiratorysignsarespo-radicallyreportedindogsbutareregularlydescribedinhumanpatientsinfectedwithhumanmonocyticehrli-chiosis(HME)[3].
Interstitialpneumoniacanhaveaninfectiousornon-infectiousetiology.
Indogs,reportedinfectiousagentsleadingtointerstitialpneumoniaareAngiostrongylusOpenAccessActaVeterinariaScandinavica*Correspondence:M.
L.
denToom@uu.
nl1DepartmentofClinicalSciencesofCompanionAnimals,FacultyofVeterinaryMedicine,UtrechtUniversity,Yalelaan108,3508TDUtrecht,TheNetherlandsFulllistofauthorinformationisavailableattheendofthearticlePage2of8Toometal.
ActaVetScand(2016)58:46vasorum,Leishmaniachagasi,Toxoplasmagondii,Pneumocystiscarinii,Babesiacanis,Leptospirasp.
,Mycoplasmasp,caninedistempervirusandadenovi-rus[4–12].
Inpatientswithinterstitialpneumonia,gasexchangeisoftenimpairedduetoventilation-perfusionmismatching,intrapulmonaryshunting,anddecreaseddiffusionacrosstheabnormalinterstitiumwitharterialhypoxiaasaconsequence.
Incontrasttothesystemicvasculaturethatrespondswitharterialvasodilationtobetterperfusehypoxictissue,thepulmonaryvasculatureconstrictsinresponsetohypoxia.
Besidespulmonaryvasoconstriction,hypoxiaalsocausesproliferationofthesmoothmusclecellsinthearterialwall.
Bothphenom-enaleadtoadecreaseinluminalcross-sectionalareaandanincreaseinpulmonaryvascularresistanceindexwithpulmonaryhypertension(PH)asaconsequence.
Pulmonaryhypertensionisclassifiedbasedontheunderlyingdiseaseanditstreatmentisaimedatimprov-ingtheclinicalsignsandaddressingtheprimarydiseaseprocess[13].
AlthoughPHisoftenirreversible,PHisreversibleinsomecasesiftheunderlyingetiologyisdiag-nosedandtreatedaccordingly.
ReversibilityofPHhasforinstancebeendemonstratedindogsaftersuccessfultreatmentforA.
vasorum[14].
Pulmonarychangesconsistentwithinterstitialpneu-moniahavebeenreportedpreviouslyinhumanswithHME[3]andasanatypicalfindingindogswithCME[15–18].
However,CMEisgenerallynotrecognizedasoneofthepossiblediseasesleadingtointerstitialpneu-moniaandsecondaryPHindogs.
OnlyonecaseofPHassociatedwithE.
canisinfectionhasbeenreportedworldwide[19].
Consequently,CMEmightbeunderdiag-nosedasapossiblecauseofinterstitialpneumoniaandsecondaryPH.
Thiscasereportdescribestheclinical,radiographicandechocardiographicpresentationofadogwithinter-stitialpneumoniaandseverePHsuspectedtobeassoci-atedwithE.
canisinfection.
CasepresentationAseven-year-old,intactmale,mixedbreeddogweigh-ing8.
1kgwaspresentedtotheEmergencyServiceoftheDepartmentofClinicalScienceofCompanionAni-malsoftheFacultyofVeterinaryMedicine,UtrechtUniversitywitha2weekshistoryoflethargy,progres-sivedyspneaandcoughing.
ThedogpreviouslylivedintheCapeVerdeanislandsforapproximately3yearsandreturnedtotheNetherlands10monthsbeforepresenta-tion.
Inthepast2years,thedoghadshowedchronicmildexerciseintoleranceandhadafewepisodesofdiarrheathatresolvedwithsymptomatictherapy.
Thedogwasup-todatewithhisvaccinationsandanthel-minthictreatments.
Physicalexaminationshowedgeneralizedweaknessanddecreasementalstate.
Cardiovascularexamina-tionrevealedtachycardia,weakperipheralpulses,palemucousmembranes,prolongedcapillaryrefilltime,jugu-lardistensionsandvenouspulses,andagradethreeoutofsixsystolicmurmurwiththepointofmaximalinten-sityovertherightcardiacapex.
Thedogwasalsoseverelydyspneicanddemonstratedharshlungsoundsonauscul-tation.
Theabdomenwasdistendedandpositiveundula-tionwasdetected.
Thesefindingswereconsistentwithpulmonarydisease,right-sidedheartfailureandpoorperipheralperfusion.
Completebloodcount(CBC)showedamoderatemicrocytic,hypochromicanemia,moderateleukocyto-siswithamarkedleftshiftandaseverethrombocyto-penia.
Biochemistryshowedseverehyperproteinemia,hyperglobulinemiaandamildhypoalbuminemia.
Serumproteinelectrophoresisshowedapolyclonalpeakinthegammaglobulinregion.
Arterialbloodgasanalysisshowedaseverehypoxemiawithhypocapnia.
Urinaly-sisshowedmildhemoglobinuria,glucosuriaandpro-teinuria.
Bloodsamplesweresubmittedforserologicalandmolecularbiologicaltesting.
Immunofluorescenceantibodytest(IFAT)forE.
canis(MegaFLUOEhrlichiacanis,MegaCorDiagnostikGmbH,Hrbranz,Aus-tria)waspositive(IgGtiter>2560),butpolymerasechainreaction(PCR)amplificationforEhrlichiagenus(real-timePCR,LightCycler2.
0,RocheDiagnosticsGmBH,Mannheim,Germany,primersusedasdescribedprevi-ously[20])wasnegative.
SerologyforLeishmaniasp.
(Dog-DAT,Leishmaniaspecificantibodydetectionkit,KoninklijkInstituutvoordeTropen,Amsterdam,theNetherlands)andB.
canis.
(MegaFLUOBabesiscanis,MegaCorDiagnostikGmbH,Hrbranz,Austria)andantigensnaptestsforA.
vasorum(AngioDetectTest,IDEXXLaboratories)andDirofilariaimmitis(SNAPHeartwormRTTest,IDEXXLaboratories)werealsoneg-ative.
LaboratoryresultsaresummarizedinTable1.
Onthoracicradiographs,amilddiffuseincreaseinpulmonaryopacitywithaninterstitiallungpatternandmildperibronchialcuffingwasseen,whichwasmostaccentuatedinthecaudodorsallunglobes.
Thinpleuralfissurelineswerenotedbetweenalllunglobes.
Thecar-diacsilhouetteshowedsignsofright-sidedcardiomegaly(vertebralheartscore(VHS):11.
0,referenceinterval75mmHg)[13],(Fig.
3).
ToaddresstheseverehypoxemiaandPHthedogwasplacedinanoxygencagewithaninspiredconcentra-tionofoxygenbetween40and50%.
Theclinicalsignsofthedogdidnotimprovemarkedlywiththeextraoxygensupplementation.
Becauseanemiacouldhavecontributedtothecardiovascularsignsandthepoortis-sueoxygenation,atypedpackedredbloodcelltransfu-sionwasadministered.
Basedonthetravelhistory,theabnormalitieswithintheCBCandbiochemicalanalysisandthepositiveserologyforE.
canis,aninfectionwithCMEwassuspected.
Treatmentwithdoxycycline(5mg/kg,orallytwicedaily)(Doxoral,ASTFarma,Oudewa-ter,theNetherlands),pimobendan(0.
3mg/kg,orallytwicedaily)(CardisureFlavour,EurovetAnimalHealthBV,Bladel,theNetherlands)andsildenafil(1.
5mg/kg,orallytwicedaily)(Viagra,Pfizer,NewYork,USA)wasinitiated.
Thehematocritincreasedfrom20to36%afterthebloodtransfusionandthedog'sclinicalconditionimprovedremarkably.
However,thedogremainedmod-eratelydyspneicandseverelyhypoxic(PaO2:46.
5mmHg,referenceinterval:85.
0–103.
3mmHg).
Thedyspneagraduallyimprovedandthedogseemedcomfortableout-sidetheoxygencageafter6daysoftreatment,althoughtheimprovementofthehypoxemiawasonlyminimal(PaO2:55mmHg,referenceinterval:85–103.
3mmHg,Table1).
Becauseoffinanciallimitationsoftheowner,thedogwasdischargedwiththeabove-mentionedthera-piesatthattime.
Seventeendaysafterinitiationoftreatment,thedogwasadmittedviathecardiologypolyclinicsofthesameuni-versityandre-examined.
Atthattime,therewascompleteresolutionofallclinicalsignsandphysicalexaminationwascompletelyunremarkable.
CBCshowednormalplate-letcountsandleukogram,withonlyaverymildmicrocytichypochromicanemia.
Biochemicalanalysisagainshowedseverehyperproteinemiaandhyperglobulinemia.
TheTable1Summaryofhaematological,biochemical,serologicalandurineandbloodgasanalysisresultsArterialbloodgasanalysiswasperformedwithaninspiredconcentrationofoxygenof21%ValuesinitalicsareoutsidethereferenceintervalMCVmeancorpuscularvolume,MCHCmeancorpuscularhemoglobinconcentration,MCHmeancorpuscularhemoglobin,WBCwhitebloodcellcount,UPCurinaryproteintocreatinineratio,PaO2partialarterialoxygenpressure,PaCO2partialarterialcarbondioxidepressure,BEbaseexcessParameterDay1Day7Day17Day50ReferenceintervalHematocrit(L/L)0.
200.
380.
400.
340.
42–0.
61MCV(fl)57.
759.
959.
963.
5–72.
9MCHC(mmol/L)21.
721.
822.
220.
5–22.
4MCH(fmol)1.
251.
311.
331.
37–1.
57TotalWBC(*109/L)23.
16.
66.
74.
5–14.
6Segmentedneutrophils(*109/L)17.
32.
64.
42.
9–11.
0Bandneutrophils(*109/L)3.
20.
00.
00.
0–0.
3Lymphocytes(*109/L)2.
13.
01.
80.
8–4.
7Monocytes(*109/L)0.
50.
40.
30.
0–0.
9Eosinophils(*109/L)0.
00.
50.
20.
0–1.
6Platelets(*109/L)15251166144–603Urea(mmol/L)4.
17.
03.
0–12.
5Creatinine(mol/L)33747750–129Sodium(mmol/L)145145141141–150Potassium(mmol/L)4.
14.
73.
73.
6–5.
6Totalprotein(g/L)911198955–72Albumin(g/L)16272626–37Gamma-globulins(g/L)5768403–9UPC0.
80.
31:25601:256040areconsideredpositiveforE.
canisexposure[21].
InFig.
3Echocardiographicimagesatpresentationfromleftapical4-chamberview.
acolorDopplermapofseveretricuspidregurgitation.
RArightatrium,RVrightventricle,LAleftatrium,LVleftventricle.
bspectralDopplertraceoftricuspidregurgitation.
Tricuspidsystolicvelocityof5.
8m/s,indi-catingapeaktricuspidpressuregradientofapproximately136mmHg,gradedasseverepulmonaryhypertension(reference75mmHgFig.
4Rightlateral(a)anddorsoventral(b)thoracicradiographs2weeksafterdischarge.
Radiographsdemonstratingresolutionofcardiomegaly(vertebralheartscore:10.
2,referenceinterval2560),whichstrength-enedthesuspicionofanactiveinfection[22].
However,definiteactiveinfectionatthetimeofpres-entationcouldnotbeproven,becausePCRamplifica-tionforEhrlichiagenuswasnegativeandanti-EhrlichialIgGantibodiespersistforseveralmonthstoyearsaftereliminationoftheparasite[23].
AnegativeresultfromaPCRtestcanoccurwhenorganismsincirculationarebelowthelevelofdetection,asmayhappenwheninfec-tionsarechronic.
IthasbeendemonstratedthatdogscanbePCRnegativeonbloodsamples,butPCRpositiveonsplenicaspirates[21].
ItishypothesizedthattheE.
canisaresequesteredinsplenicmacrophagestoavoidimmuneelimination.
Unfortunately,inthepresentcase,theown-ersdeclinedfineneedleaspiratesofthespleenduetothepotentialrisksandstressinvolved,e.
g.
internalbleeding,aggravationofthedyspnea.
Pairedserologysamplescanalsoprovideusefulinformationaboutantibodykinetics,whichmaypointtocurrentstatusofinfection.
Afour-foldincreaseinIgGantibodiesovertimeissuggestedtobeevidenceforanactiveinfection[24].
Antibodytiterswilldecreasegraduallyafterappropriatetreatment,butmaypersistformonthstoyearsevenafterfullclini-calrecovery[23,25].
Inthiscase,theEhrlichiaIgGtiterwasstillveryhigh17daysafterinitiationofdoxycyclinetherapy,probablyduetotheshorttimebetweenstartofthetreatmentandretesting;IFATwasunfortunatelynotrepeatedonday50.
Althoughdoxycyclinetherapygenerallyresultsinfastclinicalimprovementandimprovementofmostlabora-toryabnormalities,persistenceofhyperglobulinemiaisgenerallyobservedforalongerperiod.
Moststudieshaveshownnormalizationofserumproteinelectrophoresisresultsafter3–9monthsoftherapy[1,15].
Thisexplainsthepersistenceofhyperglobulinemiaatthere-examina-tionsofthedogatdays17and50.
Inhumanmedicine,respiratorysignsarecommonlydescribedasaconsequenceofHMEinfection[3]andacuterespiratorydistresssyndrome(ARDS)hasalsobeenreportedasasevere,althoughuncommon,findinginHME[26–28].
BothCMEandHMEanimalmodelsalsorevealedprominentmononuclearcellularinfiltrationintheinteralveolarsepta,endothelialdamageandvasculi-tisinthelungs[16,29].
Thiscouldexplainthepulmonarychangesfoundinthisdogandtheclinicalandradio-graphicimprovementaftertreatmentwithdoxycycline.
However,recently,acuteresolutionofpatchypulmonaryalveolarinfiltrateshasbeendescribedaftersildenafiltherapyindogswithidiopathicPHandPHsecondarytoidiopathiclungfibrosis[30].
Therefore,sildenafiltherapymightalsohavecontributedtotheimprovementoftheradiographicchangesinthiscase.
AnotherexplanationFig.
5Echocardiographicimagesobtained2weeksaftertreatmentfromrightparasternalshortaxisview.
a,b:Two-dimensional(a)andM-mode(b)viewdemonstratingnormalizationofcardiacdimensionsandfunction.
cTwo-dimensionalviewofpulmonaryartery(PA)andaorta(AO).
ThePAisuniformlyminimallydilatedwithaPA/Aoratioof1.
2(referenceinterval:0.
8–1.
15)Page7of8Toometal.
ActaVetScand(2016)58:46fortheradiographicabnormalitiesandtheimprovementondoxycyclinetherapythatcannotbeexcludedisthatthedogsufferedfromabacterialpneumonia.
Furthermore,animportantpossiblefactorthatmighthavecontributedtothehypoxemiaandPHinthisdogispulmonarythromboembolism(PTE)[31].
PTEcanoccurascomplicatingsequelaeinpatientswithPHorcanbetheprimarycauseofPH[32].
Inpeople,itisincreasinglyrecognizedthatpatientswithpulmonaryarterialhypertensionhavedysregulatedcoagulationandantithrombotichomeostasis,whichmaycontributetoaprothromboticstate[33].
Unfortunately,wedidnotperformdiagnosticinvestigationssuchasD-dimercon-centration[34],computedtomographypulmonaryangi-ography[35]orthromboelastography(TEG)[36,37]toinvestigateifthedogsufferedfromPTEoraprothrom-boticstate.
However,totheauthor'sknowledge,PTEhasneverbeenassociatedwithCMEinveterinaryliterature.
OnlytwocasesofaorticandportalveinthrombosishavebeendescribedindogswithCME[38,39].
TreatmentofPHisaimedateliminatingorimprovingtheunderlyingdiseaseprocess.
IfthePHisnotcontrolledbyprimarydiseasetherapyorifthePHisidiopathic,treatmentwithpulmonaryarterialdilatorsmaybeimple-mented.
Inveterinarymedicinecurrently,onlyphos-phodiesteraseinhibitorsareused.
Sildenafilisahighlyselectivephosphodiesterasefiveinhibitorthathasbeenusedinveterinarymedicinewithencouragingresults[30,40].
Pimobendan,acalcium-sensitizingagentwithphosphodiesterasethreeinhibitingactionshasalsobeenused,especiallywhenleftheartdiseaseisacontributingcause[41].
Inthepresentcase,adualtherapywithpul-monaryarterialdilatorswasinitiated,becausewehopedthiswouldamelioratetheveryseverePHandclinicalsignsfasterthanamonotherapywithsildenafil.
Althoughrecoveryhasbeendescribedinasimilarcasewithjustamonotherapywithdoxycycline[19],webelievethatthesymptomaticsupportwithpulmonaryvasodilatorswasjustifiedinthisdog.
MildtomoderateimprovementoftricuspidregurgitationgradientbysildenafiltherapyhasbeendescribedinsomedogswithPH[30],butnotinothers[42].
Consequently,wecannotruleoutthattheimprovementoftheechocardiographicchangescouldalsobepartiallyexplainedbytheuseofthevasodilatingdrugs.
Ideally,anotherechocardiogramshouldhavebeenperformedafterdiscontinuationofthevasodilatorther-apy.
However,theimprovementwassodramatic,thatwedonotbelievethatthiscouldbesolelyexplainedbythevasodilatortherapy.
ThiscasereportillustratesthatCMEmightbeasso-ciatedwithsignificantpulmonarydiseaseandthatitshouldbeconsideredasapossibledifferentialdiag-nosisindogspresentingwithdyspneaandsecondarypulmonaryhypertension,especiallyindogsthathavebeeninendemicareas.
ThisisimportantbecauseCMEisatreatablediseaseanditslungandcardiacmanifesta-tionsmaybecompletelyreversible.
Authors'contributionsCVperformedtheinitialclinicalinvestigationsofthedogandwasresponsibleforthecareandtreatmentofthedogduringadmittanceattheIntensiveCareUnit.
EBwasresponsiblefortheserologicalandmolecularbiologicaldiagnostictesting.
MDTalsoperformedclinicalinvestigationsofthedogandperformedandevaluatedtheechocardiogramsofthedogduringhospitaliza-tionandatfollow-up.
TDperformedandevaluatedtheinitialechocardiogramofthedogatpresentationandwasresponsiblefortheinterpretationofthethoracicradiography.
ThemanuscriptwasdraftedbyMDTandfinalizedjointlybyallauthors.
Allauthorsreadandapprovedthefinalmanuscript.
Authordetails1DepartmentofClinicalSciencesofCompanionAnimals,FacultyofVeterinaryMedicine,UtrechtUniversity,Yalelaan108,3508TDUtrecht,TheNetherlands.
2DepartmentofDiagnosticImaging,FacultyofVeterinaryMedicine,UtrechtUniversity,Yalelaan108,3508TDUtrecht,TheNetherlands.
3DepartmentofInfectiousDiseasesandImmunology,FacultyofVeterinaryMedicine,Utre-chtUniversity,POBox80.
165,3508TDUtrecht,TheNetherlands.
CompetinginterestsTheauthorsdeclarethattheyhavenocompetinginterests.
Received:19March2016Accepted:30June2016References1.
Sainz,RouraX,MiróG,EstradaPeaA,KohnB,HarrusS,etal.
GuidelineforveterinarypractitionersoncanineehrlichiosisandanaplasmosisinEurope.
ParasitVectors.
2015;8:75.
2.
LittleSE.
Ehrlichiosisandanaplasmosisindogsandcats.
VetClinNorthAmSmallAnimPract.
2010;40:1121–40.
3.
EngTR,HarkessJR,FishbeinDB,DawsonJE,GreeneCN,RedusMA,etal.
Epidemiologic,clinical,andlaboratoryfindingsofhumanehrlichiosisintheUnitedStates,1988.
JAMA.
1990;264:2251–8.
4.
PandherK,PodellB,GouldDH,JohnsonBJ,ThompsonS.
Interstitialpneumoniainneonatalcaninepupswithevidenceofcaninedistempervirusinfection.
JVetDiagnInvest.
2006;18:201–4.
5.
GonalvesR,TafuriW,deMeloM,RasoP.
Chronicinterstitialpneumo-nitisindogsnaturallyinfectedwithLeishmania(Leishmania)chagasi:ahistopathologicalandmorphometricstudy.
RevInstMedTropSaoPaulo.
2003;45:153–8.
6.
KirbergerRM,LobettiRG.
RadiographicaspectsofPneumocystiscariniipneumoniaintheminiatureDachshund.
VetRadiolUltrasound.
1998;39:313–7.
7.
HongS,KimO.
MolecularidentificationofMycoplasmacynosfromlaboratorybeagledogswithrespiratorydisease.
LabAnimRes.
2012;28:61–6.
8.
GendronK,ChristeA,WalterS,SchweighauserA,FranceyT,DoherrMG,etal.
SerialCTfeaturesofpulmonaryleptospirosisin10dogs.
VetRec.
2014;174:169.
9.
DasteT,LucasM,AumannM.
Cerebralbabesiosisandacuterespiratorydistresssyndromeinadog.
JVetEmergCritCare.
2013;23:615–23.
10.
BorgeatK,SudunaguntaS,KayeB,SternJ,LuisFuentesV,ConnollyDJ.
Retrospectiveevaluationofmoderate-to-severepulmonaryhypertensionindogsnaturallyinfectedwithAngiostrongylusvasorum.
JSmallAnimPract.
2015;56:196–202.
11.
CastlemanWL.
Bronchiolitisobliteransandpneumoniainducedinyoungdogsbyexperimentaladenovirusinfection.
AmJPathol.
1985;119:495–504.
12.
CapenCC,ColeCR.
Pulmonarylesionsindogswithexperimentalandnaturallyoccurringtoxoplasmosis.
PatholVet.
1966;3:40–63.
Page8of8Toometal.
ActaVetScand(2016)58:4613.
KellihanH,StepienR.
Pulmonaryhypertensionindogs:diagnosisandtherapy.
VetClinNorthAmSmallAnimPract.
2010;40:623–41.
14.
EstèvesI,TessierD,DandrieuxJ,PolackB,CarlosC,BoulangerV,etal.
Reversiblepulmonaryhypertensionpresentingsimultaneouslywithanatrialseptaldefectandangiostrongylosisinadog.
JSmallAnimPract.
2004;45:206–9.
15.
NeerTM,BreitschwerdtE,GreeneR,LappinM.
ConsensusstatementonehrlichialdiseaseofsmallanimalsfromtheinfectiousdiseasestudygroupoftheACVIM.
AmericanCollegeofVeterinaryInternalMedicine.
JVetInternMed.
2002;16:309–15.
16.
SotomayorEA,PopovVL,FengHM,WalkerDH,OlanoJP.
Animalmodeloffatalhumanmonocytotropicehrlichiosis.
AmJPathol.
2001;158:757–69.
17.
FrankJR,BreitschwerdtEB.
Aretrospectivestudyofehrlichiosisin62dogsfromNorthCarolinaandVirginia.
JVetInternMed.
1999;13:194–201.
18.
CodnerEC,RobertsRE,AinsworthAG.
Atypicalfindingsin16casesofcanineehrlichiosis.
JAmVetMedAssoc.
1985;186:166–9.
19.
LocatelliC,StefanelloD,RiscazziG,BorgonovoS,ComazziS.
PulmonaryhypertensionassociatedwithEhrlichiacanisinfectioninadog.
VetRec.
2012;170:676.
20.
BekkerCPJ,deVosS,TaoufikA,SparaganoOAE,JongejanF.
SimultaneousdetectionofAnaplasmaandEhrlichiaspeciesinruminantsanddetectionofEhrlichiaruminantiuminAmblyommavariegatumticksbyreverselineblothybridization.
VetMicrobiol.
2002;89:223–38.
21.
HarrusS,WanerT.
Diagnosisofcaninemonocytotropicehrlichiosis(Ehrli-chiacanis):anoverview.
VetJ.
2011;187:292–6.
22.
WenB,RikihisaY,MottJM,GreeneR,KimHY,ZhiN,etal.
ComparisonofnestedPCRwithimmunofluorescent-antibodyassayfordetectionofEhrlichiacanisinfectionindogstreatedwithdoxycycline.
JClinMicrobiol.
1997;35:1852–5.
23.
BartschRC.
Post-therapyantibodytitersindogswithehrlichiosis:follow-upstudyon68patientstreatedprimarilywithtetracyclineand/ordoxycycline.
JVetInternMed.
1996;10:271–4.
24.
WanerT,HarrusS,JongejanF,BarkH,KeysaryA,CornelissenAW.
Signifi-canceofserologicaltestingforehrlichialdiseasesindogswithspecialemphasisonthediagnosisofcaninemonocyticehrlichiosiscausedbyEhrlichiacanis.
VetParasitol.
2001;95:1–15.
25.
IqbalZ,RikihisaY.
ReisolationofEhrlichiacanisfrombloodandtissuesofdogsafterdoxycyclinetreatment.
JClinMicrobiol.
1994;32:1644–9.
26.
WeaverRA,VirellaG,WeaverA.
Ehrlichiosiswithseverepulmonarymani-festationsdespiteearlytreatment.
SouthMedJ.
1999;92:336–9.
27.
PatelRG,ByrdMA.
Nearfatalacuterespiratorydistresssyndromeinapatientwithhumanehrlichiosis.
SouthMedJ.
1999;92:333–5.
28.
MutnejaR,ShahM,ShivamurthyP,GowaniS,DelgadoColonD,LawlorM.
Acuterespiratorydistresssyndromeinhumangranulocyticehrlichiosis.
ConnMed.
2014;78:345–7.
29.
ReardonMJ,PierceKR.
Acuteexperimentalcanineehrlichiosis.
II.
Sequen-tialreactionofthehemicandlymphoreticularsystemofselectivelyimmunosuppresseddogs.
VetPathol.
1981;18:384–95.
30.
KellihanH,WallerK,PinkosA,SteinbergH,BatesM.
Acuteresolutionofpulmonaryalveolarinfiltratesin10dogswithpulmonaryhypertensiontreatedwithsildenafilcitrate:2005–2014.
JVetCardiol.
2015;17:182–91.
31.
GoggsR,BenigniL,FuentesV,ChanD.
Pulmonarythromboembolism.
JVetEmergCritCare.
2009;19:30–52.
32.
GalieN,HumbertM,VachieryJL,GibbsS,LangI,TorbickiA,etal.
2015ESC/ERSGuidelinesforthediagnosisandtreatmentofpulmonaryhyper-tension:thejointtaskforceforthediagnosisandtreatmentofpulmonaryhypertensionoftheEuropeansocietyofcardiology(ESC)andtheEuropeanrespiratorysociety(ERS):endorsedby:associationforEuropeanpaediatricandcongenitalcardiology(AEPC),Internationalsocietyforheartandlungtransplantation(ISHLT).
EurHeartJ.
2016;37:67–119.
33.
RoldanT,LandzbergMJ,DeicicchiDJ,AtayJK,WaxmanAB.
Anticoagula-tioninpatientswithpulmonaryarterialhypertension:anupdateoncurrentknowledge.
JHeartLungTransplant.
2016;35:151–64.
34.
EpsteinSE,HopperK,MellemaMS,JohnsonLR.
DiagnosticutilityofD-dimerconcentrationsindogswithpulmonaryembolism.
JVetInternMed.
2013;27:1646–9.
35.
GoggsR,ChanDL,BenigniL,HirstC,KellettGregoryL,FuentesVL.
Comparisonofcomputedtomographypulmonaryangiographyandpoint-of-caretestsforpulmonarythromboembolismdiagnosisindogs.
JSmallAnimPract.
2014;55:190–7.
36.
GoggsR,WiinbergB,Kjelgaard-HansenM,ChanDL.
Serialassessmentofthecoagulationstatusofdogswithimmune-mediatedhaemolyticanaemiausingthromboelastography.
VetJ.
2012;191:347–53.
37.
KolA,BorjessonDL.
Applicationofthrombelastography/thromboelasto-metrytoveterinarymedicine.
VetClinPathol.
2010;39:405–16.
38.
BresslerC,HimesLC,MoreauRE.
PortalveinandaorticthrombosesinaSiberianhuskywithehrlichiosisandhypothyroidism.
JSmallAnimPract.
2003;44:408–10.
39.
LambCR,WrighleyRH,SimpsonKW,HijfteMF,GardenOA,SmythJBA,etal.
Ultrasonographicdiagnosisofportalveinthrombosisinfourdogs.
VetRadiolUltrasoun.
1996;37:121–9.
40.
BrownAJ,DavisonE,SleeperMM.
Clinicalefficacyofsildenafilintreat-mentofpulmonaryarterialhypertensionindogs.
JVetInternMed.
2010;24:850–4.
41.
AtkinsonKJ,FineDM,ThombsLA,GorelickJJ,DurhamHE.
EvaluationofpimobendanandN-terminalprobrainnatriureticpeptideinthetreat-mentofpulmonaryhypertensionsecondarytodegenerativemitralvalvediseaseindogs.
JVetInternMed.
2009;23:1190–6.
42.
KellumH,StepienR.
Sildenafilcitratetherapyin22dogswithpulmonaryhypertension.
JVetInternMed.
2007;21:1258–64.
美国Cera 2核4G 20元/45天 香港CN2 E5 20M物理机服务器 150元 日本CN2 E5 20M物理机服务器 150元 提速啦
提速啦 成立于2012年,作为互联网老兵我们一直为用户提供 稳定 高速 高质量的产品。成立至今一直深受用户的喜爱 荣获 “2021年赣州安全大赛第三名” “2020创新企业入围奖” 等殊荣。目前我司在美国拥有4.6万G总内存云服务器资源,香港拥有2.2万G总内存云服务器资源,阿里云香港机房拥有8000G总内存云服务器资源,国内多地区拥有1.6万G总内存云服务器资源,绝非1 2台宿主机的小商家可比。...

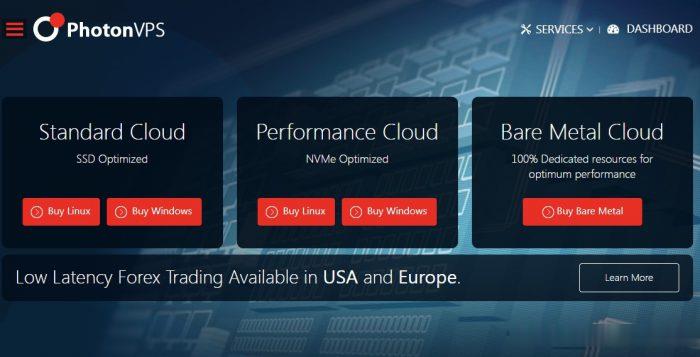
PhotonVPS:美国Linux VPS半价促销2.5美元/月起,可选美国洛杉矶/达拉斯/芝加哥/阿什本等四机房
photonvps怎么样?photonvps现在针对旗下美国vps推出半价促销优惠活动,2.5美元/月起,免费10Gbps DDoS防御,Linux系统,机房可选美国洛杉矶、达拉斯、芝加哥、阿什本。以前觉得老牌商家PhotonVPS贵的朋友可以先入手一个月PhotonVPS美国Linux VPS试试了。PhotonVPS允许合法大人内容,支持支付宝、paypal和信用卡,30天退款保证。Photo...
Boomer.Host(年付3.5美)休斯敦便宜VPS
Boomer.Host是一家比较新的国外主机商,虽然LEB自述 we’re now more than 2 year old,商家提供虚拟主机和VPS,其中VPS主机基于OpenVZ架构,数据中心为美国得克萨斯州休斯敦。目前,商家在LET发了两款特别促销套餐,年付最低3.5美元起,特别提醒:低价低配,且必须年付,请务必自行斟酌确定需求再入手。下面列出几款促销套餐的配置信息。CPU:1core内存:...
cv狗狗为你推荐
宿迁服务器租用 域名备案号查询 yardvps windows主机 站群服务器 哈喽图床 174.127.195.202 监控宝 godaddy域名转出 512m内存 网站挂马检测工具 ibox官网 100x100头像 免费吧 服务器合租 美国独立日 空间登入 下载速度测试 西安主机 阿里云邮箱申请 更多